Day One of the 7th Congress of the Asia-Pacific Glaucoma Society (APGC 2024) in Manila, Philippines kicked off with a symposium on optimizing medical therapy for glaucoma treatment. Leading experts from around the world highlighted the importance of personalized approaches, fixed-combination medicines, and innovative drug delivery systems.
Choosing the best first-line medicine
Dr. Manchima Makornwattana from Thammasat University, Thailand emphasized that the ‘best’ medication isn’t one-size-fits-all but depends on several factors unique to each patient.
So, what makes a drug the best choice? According to Dr. Makornwattana, it boils down to the four C’s: convenience, comfort, compliance, and cost.
- Convenience: The medication should fit seamlessly into the patient’s daily routine. A drug that’s easy to administer is more likely to be used consistently.
- Comfort: Patients need a medication that doesn’t cause discomfort or adverse side effects. Eye drops that irritate or cause allergies are a no-go.
- Compliance: For treatment to be effective, patients must stick with it. This means choosing a medication that the patient can and will use regularly.
- Cost: Finally, the drug must be affordable, ideally covered by insurance. If a patient can’t afford their medication, they won’t be able to keep up with their treatment.

Dr. Makornwattana shared anecdotes to illustrate her points. One patient, she noted, couldn’t use a particular eye drop because it required refrigeration, and he had no fridge at home. Another struggled with small print on medication labels due to poor eyesight—a common issue among glaucoma patients.
She also discussed alternatives like selective laser trabeculoplasty (SLT), which can control eye pressure with fewer side effects and lower long-term costs.
“The best medicine for everyone may not be the same,” she concluded. “Consider convenience, comfort, compliance, and cost to find the most appropriate treatment for each patient.”
When to switch and when to add medications
Dr. Catherine Liu from National Yang Ming Chiao Tung University in Taiwan offered insights on managing primary open-angle glaucoma (POAG) and ocular hypertension.
For many patients, the first line of defense against glaucoma is monotherapy, but it’s not always a perfect fit. “There are instances where we have to switch to another medication due to drug intolerance or lack of effectiveness,” Dr. Liu explained.
An intriguing study she mentioned involved geriatric patients with glaucoma. After switching from beta-blockers to brimonidine, these patients not only experienced better IOP control but also reported increased energy levels.1
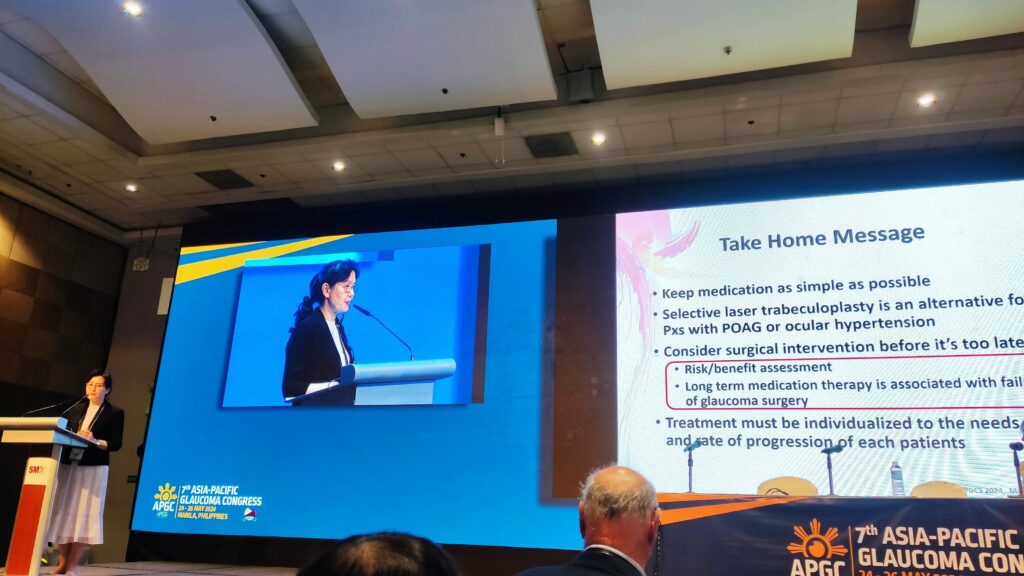
Dr. Liu also discussed the advantages of combination therapies, such as combining a prostaglandin analogue with a beta blocker, which can enhance IOP reduction while maintaining ease of use for patients.
Beyond medications, Dr. Liu urged her colleagues to consider laser and surgical interventions. “SLT is a great alternative for patients with POAG or ocular hypertension,” she said. “And don’t wait too long to consider surgery. It’s important to weigh the risks and benefits and act before it’s too late.”
The case for preservative-free eye drops
Dr. Anton Hommer from Austria discussed the impact of preservatives in glaucoma medications, particularly benzalkonium chloride (BAK). He explained that while preservatives prevent microbial contamination, they can also cause significant side effects like dry eye, redness, and discomfort.
Dr. Hommer briefly listed preservative-free medications that have been shown to be just as effective in lowering IOP without causing ocular surface disease. He also noted a shift in guidelines towards preservative-free formulations.

According to Dr. Hommer, there’s been a notable rise in the prescription of preservative-free medications in Austria and Europe. “By 2023, more than 40% of patients were receiving preservative-free eye drops,” he stated, marking a significant jump from previous years.
Dr. Hommer’s concluding message was clear and unequivocal: “So, my answer is yes, we need preservative-free eye drops for most patients.”
Tackling adherence issues
Dr. Mimiwati Zahari from the University of Malaya in Malaysia addressed medication adherence, a critical issue in glaucoma treatment. She pointed out that glaucoma’s asymptomatic nature makes it challenging for patients to recognize the importance of adhering to their treatment.
Dr. Zahari categorized adherence barriers into four groups: provider-related, patient-related, medication-related, and situational/environmental factors. She emphasized the need for continuous adherence rather than “white coat compliance,” where patients only adhere to their regimen before doctor visits.
“Explain what the disease is, why treatment is needed, and how the drugs work,” she advised. Simplifying regimens, involving family members, and using reminder systems can improve adherence.
Dr. Zahari also discussed promising developments in non-topical drug delivery systems, such as sustained-release implants like Durysta (Allergan; California, USA) and iDose (Glaukos; California, USA), which could significantly reduce the burden of daily eye drop regimens.
The power of fixed-combination medications
Dr. Widya Artini Ikke Sumantri from JEC Eye Hospital in Indonesia then highlighted the benefits of fixed-combination regimens in glaucoma therapy. She explained that many glaucoma patients, especially those with ocular hypertension, often require multiple medications to control IOP.
“It’s not unusual for these patients to require multiple medications,” she explained. “Fixed-combination treatments simplify this process, making it easier and more convenient”
Fixed combinations improve usability, enhance patient adherence, and reduce adverse events associated with preservatives in individual eye drops. Dr. Sumantri noted that about 80% of patients in one study struggled with complex regimens.2
She highlighted that combinations like latanoprost and timolol are more effective and have fewer adverse events compared to individual agents. Dr. Sumantri also discussed newer fixed-combination therapies, such as those involving ROCK inhibitors.
Exploring maximum tolerated medical therapy
Dr. Prin Rojanapongpun of the Eye Care Center at MedPark Hospital in Thailand provided an overview of the evolving maximum tolerated medical therapy (MTMT). He defined MTMT as the pursuit of the best possible therapeutic outcome with fixed combination medications while minimizing adverse effects and addressing patient compliance challenges.
“The goal,” he said, “is to find the sweet spot where we achieve effective IOP reduction without overwhelming the patient with side effects or a cumbersome medication regimen.”
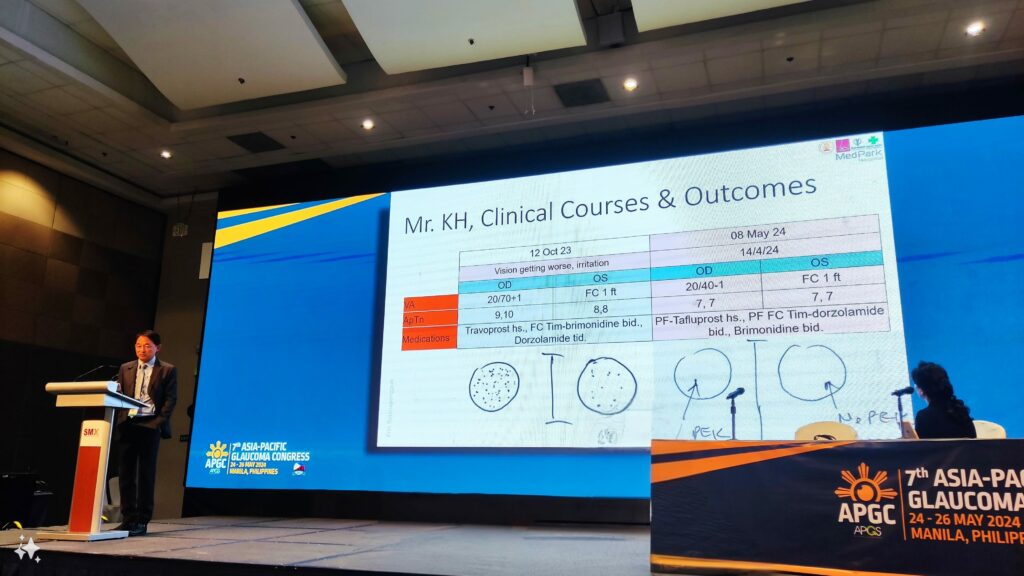
Dr. Rojanapongpun shared results from clinical trials showing the superiority of three-drug combination regimens over two-drug regimens in lowering 24-hour IOP. He emphasized a patient-centered approach and shared a case study where switching to preservative-free formulations improved a patient’s comfort and vision.3,4,5
“The data is clear,” he said. “Triple fixed combinations outperform their two-drug counterparts in both efficacy and tolerability. This can potentially transform MTMT and help prevent glaucoma progression more effectively.”
Looking ahead, he discussed emerging trends in MTMT, including quadruple fixed combinations and new drug classes like ROCK inhibitors, which promise better control of IOP with fewer side effects.
Editor’s Note: Reporting for this event took place during the 7th Congress of the Asia-Pacific Glaucoma Society (APGC 2024), held from May 24-26, 2024.
References
- Noecker RJ; Study Group for the Efficacy of Brimonidine in Geriatric Patients. Brimonidine .2% as a replacement for beta blockers in geriatric patients with glaucoma. Adv Ther. 2002;19(2):91-97.
- Sleath B, Robin AL, Covert D, Byrd JE, Tudor G, Svarstad B. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113(3):431-436.
- Baiza-Duran LM, Llamas-Moreno JF, Ayala-Barajas C. Comparison of timolol 0.5% + brimonidine 0.2% + dorzolamide 2% versus timolol 0.5% + brimonidine 0.2% in a Mexican population with primary open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2012;6:1051-1055.
- Baiza-Duran LM, Alvarez-Delgado J, Contreras-Rubio AY, et al. The efficacy and safety of two fixed combinations: timolol-dorzolamide-brimonidine versus timolol-dorzolamide. A prospective, randomized, double-masked, multi-center, 6-month clinical trial. Ann Ophthalmol. 2009;41(3-4):174-178.
- Garcia-Lopez A, Paczka JA, Jimenez-Roman J, et al. Efficacy and tolerability of fixed-combination bimatoprost/timolol versus fixed-combination dorzolamide/brimonidine/timolol in patients with primary open-angle glaucoma or ocular hypertension: a multicenter, prospective, crossover study. BMC Ophthalmol. 2014;14:161.



