APGC 2024 is officially on, and attendees at the opening ceremony were treated to a salvo of award lectures from some of the region’s current and future glaucoma luminaries.
The eyes of the ophthalmic world have shifted to Manila for the 7th Congress of the Asia-Pacific Glaucoma Society (APGC 2024), which officially kicked off on May 24. The conference’s opening day was stuffed full of symposia and sessions on some of the hottest topics in glaucomatous disease—but none with such fanfare and anticipation as the opening ceremony and award lectures at the first plenary session of the Congress.
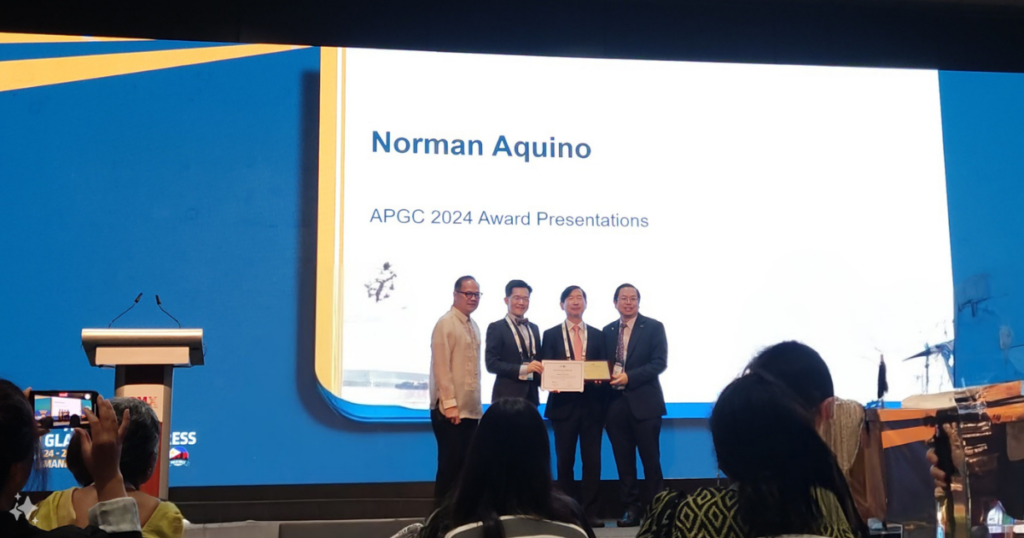
The procession of leaders in Asia-Pacific glaucoma began with Congress Chair Dr. Norman Aquino (PHL), who was joined in giving a warm mabuhay to the over 1,000 delegates at APGC 2024 by Asia-Pacific Glaucoma Society (APGS) President Dr. Seng Kheong Fan (Malaysia), Philippine Academy of Ophthalmology President Dr. Mary Ellen Sy, and Philippine Glaucoma Society President Dr. Maria Margarita Lat-Luna.
After this generous extension of Filipino hospitality, however, it was time for the main event—a barrage of the glaucoma science and knowledge that drew attendees from over 20 countries to the SMX Convention Center in Manila. And what followed was a post-lunch smorgasbord of cutting-edge science, enlightening philosophical approaches to glaucoma and life, and the beginning of a revolution in treatment of the disease.

Bridging the past and future of glaucoma
Prof. Clement Tham (Hong Kong), chair of the Award Committee and president-elect of the APGS, took the mic first to introduce the day’s first award lecture, the APGS International Award.
Given to a distinguished glaucoma specialist outside of the Asia-Pacific region for lifetime contributions, the 2024 Award was presented to the Bascom Palmer Eye Institute’s (Miami, Florida, USA) Dr. Paul Palmberg, whose talk focused on building—and being—a bridge in life and eye care.
“Each of us is potentially a bridge in several ways,” said Dr. Palmberg. “Certainly between your parents and your children—but also between your mentors and the people that you mentor, including your patients, who need you to mentor them.”
“What moves along these bridges? With your family, it’s your genes, opportunity, inheritance, language, religion, and culture,” he continued. “And from your mentors, it’s clinical skills, but also strategies, ethical behavior and modeled creativity. And this creativity is really important for your organic progress, and to your patients.”
Dr. Palmberg then reflected on his career building bridges, both as an early-career researcher exploring diabetes and diabetic retinopathy and later as a glaucoma specialist and sought-after instructor of surgical and clinical techniques in ophthalmology.
He also shared his thoughts on using failure to build bridges in knowledge. “All my work on human trabecular meshwork failed,” he said. “I couldn’t grow [human trabecular meshwork cells], but I could teach the culture work to do it. And as a result, I made changes to corneal transplant media.”
After more reflection on these bridge-building experiences over his illustrious career, Dr. Palmberg left the audience with a final thought—and perhaps one that has had the most influence on a life spent dedicated to improving human health and sight: “Don’t forget to have fun.”
Normal tension glaucoma takes the stage
Normal tension glaucoma (NTG) is a topic near and dear to the Asia-Pacific region, where incidence rates are notoriously high. In the APGS 2024 Asia-Pacific Award Lecture, honoree Dr. Ki Ho Park presented a review of the research on this silent thief of sight and the factors involved in its pathogenesis.
He began with an overview of current knowledge on the effect of mean IOP and IOP fluctuations on NTG. Of particular interest was his 2013 study that showed 12-year follow up data from Korea, which demonstrated a greater cumulative probability (p=0.012 by Log rank test) of non-progression for the upper tertile of followed patients (those showing >22% IOP reduction from baseline) than the lower (<13% reduction from baseline).1
For the influence of IOP fluctuations on NTG, Dr. Park again surveyed the existing literature on the impact of both short- and long-term fluctuations. He touched on a variety of factors influencing these fluctuations, including sleeping position. He also went deep on optic disc hemorrhages, an indicator of glaucoma progression, and the influence of factors like temperature and season, trabeculectomy, and laminar disinsertions on them.
The most recent work he referenced was on the influence of optical disc hemorrhage size on visual field progression, where he found that larger disc hemorrhages were associated with faster progression of glaucomatous disease.2
With over ten papers surveyed over the course of his talk, Dr. Park came to his conclusion about our current understanding of NTG. “Intraocular pressure and intraocular fluctuations are a risk factor for normal tension glaucoma,” he said. “Disc hemorrhage and peripapillary atrophy are associated with IOP as well.
“And finally, lamina cribrosa and peripapillary tissue biomechanical properties associated with glaucoma are also associated with IOP factors, disc hemorrhage and peripapillary atrophy.”
A revolution in primary angle closure glaucoma
For anyone working in glaucoma, the late South African Prof. Anthony Molteno and his unmatched contributions to modern glaucoma need no introduction—right on up to the glaucoma drainage device that bears his name.
APGC 2024 marked the inaugural Anthony Molteno Lecture, a series established to honor his outsized lifetime contributions toward advancing glaucoma care and surgery. The first awardee was Prof. Xiulan Zhang (China) and her celebrated 35-year career in ophthalmic clinical practice, teaching and research.
True to the disruptive spirit of innovation of Prof. Molteno, Prof. Zhang did not shy away from making a bold statement with her turn at the podium. She presented on what she believes is an impending microinvasive glaucoma surgery (MIGS) revolution in primary angle closure glaucoma (PACG).
“Trabeculectomy or phacotrabeculectomy are currently the first choice for PACG, but not an ideal surgery,” she said, pointing to filtering bleb scarring, large and thin-walled blebs, leaking wounds, infection, and choroidal detachment and hemorrhages, among other possible adverse adverse events resulting from these procedures.
Dr. Xiulan then demonstrated why she thinks MIGS procedures are possible in even advanced PACG, giving an overview of the prospects of what she termed phacogoniotomy [phacoemulsification with IOL implantation combined with goniosynechialysis (GSL) and goniotomy (GT)] and surgical peripheral iridectomy (SPI) with GSL and GT.
In Dr. Xiulan’s opinion, these two techniques are poised to become the standard of care in all stages of PACG, from early to advanced.
She went on to introduce a potentially groundbreaking new consensus for PACG with MIGS. For early cases, she proposed laser peripheral iridotomy or SPI for patients without cataracts, and phacoemulsification with IOL implantation for those with cataracts.
And in perhaps the most eyebrow-raising research she presented, she proposed the SPI, GSL and GT combination as a wholesale replacement for trabeculectomy in patients without cataracts, and phacogoniotomy for patients with cataracts.
“We believe that these new combination surgeries can bring new options and innovation into PACG in the future,” she said. “The future of PACG is being revolutionized. Trabeculectomy and phacotrabeculectomy will be replaced.”
A sneak peek at the future of glaucoma care
The award lecture extravaganza was given a fitting end with the final talk, the Manuel Aguito Lecture delivered by Prof. Paul Healey. He delved into the future of glaucoma unfolding in front of our very eyes with personalized care and polygenic risk score (PRS) testing.
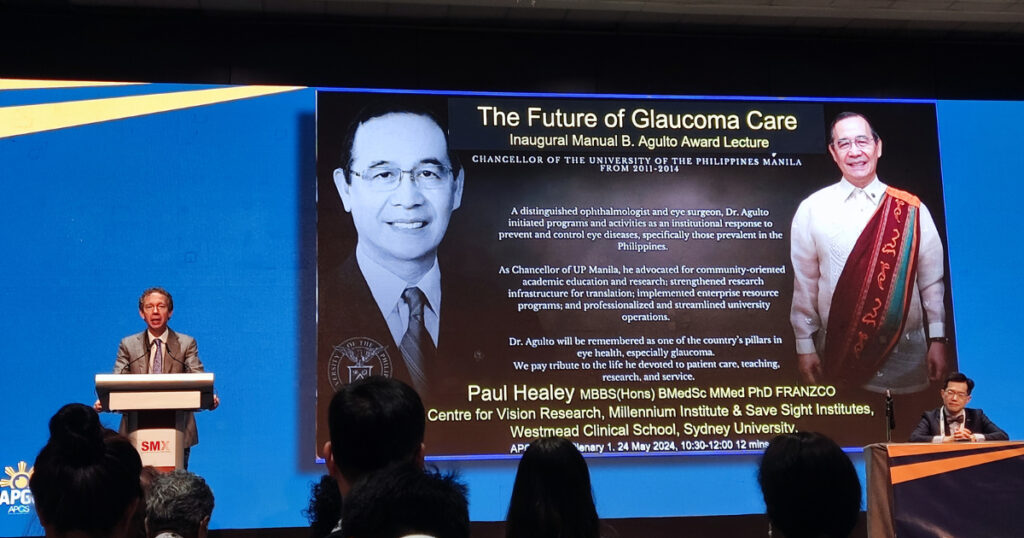
According to Prof. Healey, current issues in personalized glaucoma care include intensive expert participation in risk assessment, which currently only provides IOP guidance targets and does not perform well as a screening tool in the critical early stages of the disease.
PRS testing can fill these gaps by using genomic information to assess factors associated with the likelihood of progression and an apoptic event in response to stress. According to Prof. Healey, this opens up the door to new therapeutic targets for glaucoma.
He identified blocking apoptosis pathways with FAS-blocking drugs, introducing molecular chaperones like phenylbutyrate and trimethylamine N-oxide to enhance protein folding, and the support and enhancement of homeostasis and cell survival as potential targets that could leverage this new information.
In the end, however, he addressed the crowd with a deceptively simple exhortation to the assembled specialists on the future of glaucomatous disease treatment and management. “None of what I have shown you is the future of glaucoma care,” he said. “You are the future of glaucoma care.”
Editor’s Note: Reporting for this event took place during the 7th Congress of the Asia-Pacific Glaucoma Society (APGC 2024), held from May 24-26, 2024 in Manila, Philippines. During this session, Dr. Dewang Angmo (India) was also presented with the APGS Young Investigator Award.
References
- Kim M, Kim DM, Park KH, Kim TW, Jeoung JW, Kim SH. Intraocular pressure reduction with topical medications and progression of normal-tension glaucoma: a 12-year mean follow-up study. Acta Ophthalmol. 2013;91(4):e270-5.
- Jeong Y, Bak E, Jang M, et al. Clinical Significance of Optic Disc Hemorrhage Size in Visual Field Progression in Glaucoma. Am J Ophthalmol. 2024;263:109-116.



