In this enlightening Chinese symposium on Day 1 of the 36th Annual Meeting of the Asia-Pacific Association of Cataract and Refractive Surgeons (APACRS 2024), experts delved into the intricacies of managing presbyopia and refractive anomalies, as well as optimizing outcomes in refractive surgery.
The current situation and challenges in presbyopia treatment
First speaker Dr. Bi Hongsheng (Affiliated Eye Hospital of Shandong University of Traditional Chinese Medicine, China) highlighted the pressing issue of a surge in presbyopia patients globally due to aging. This trend holds significant clinical and social implications for further research into the mechanisms and correction methods of presbyopia.
Dr. Bi reminded delegates that presbyopia commonly begins at age 38 and reaches its peak between age 42 and 44; and that the incidence of presbyopia in people over age 52 is close to 100%. According to Dr. Bi, China has 390 million people with presbyopia and about 67.85% of them did not receive appropriate treatment due to lack of awareness.
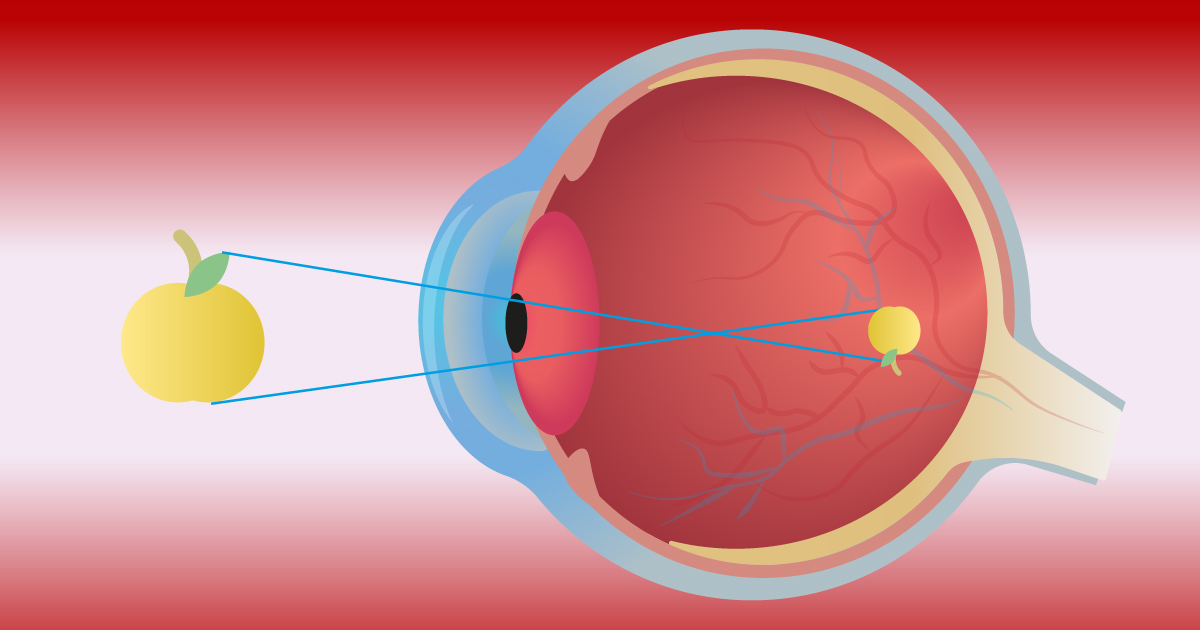
“Ideally, presbyopia treatment should achieve several objectives: restoring the diopter range of accommodation to a pre-presbyopia state, enabling smooth and rapid focusing post-treatment, maintaining the adjustment range without further intervention and ensuring normal refractive status for distance vision,” explained Dr. Bi.
Furthermore, Dr. Bi emphasized the range of available presbyopia treatments, which can be categorized into non-surgical options (such as glasses and contact lenses), surgical interventions (including corneal, intraocular or scleral surgery) and medication (such as miotic agents or drugs aimed at restoring lens elasticity). He stressed the importance of physicians strictly controlling treatment indications and offering personalized solutions based on individual examination results and needs.
“The ultimate goal of presbyopia treatment is to restore normal accommodation through various technologies and solutions, thereby providing a ‘youthful future’ for presbyopia patients,” concluded Dr. Bi.
Unlocking the enigma of refractive anomalies postoperatively
Next, Dr. Luo Lixia (Zhongshan Eye Center of Sun Yat-sen University, China) addressed the mystery behind unexpected refractive anomalies following laser-assisted in situ keratomileusis (LASIK) or cataract surgery.
According to Dr. Luo, investigation should be made into the source of these ‘refractive accidents’ — whether there are biological measurement errors (such as axis and corneal curvature) or IOL measurement errors. “One should also investigate whether the IOL is centrally positioned, and whether there is edema in the macular area,” she added.
Reflections on refractive anomalies post-cataract surgery prompt questions regarding the eccentricity of corneal cutting and the magnitude of the Kappa (K) angle. “Attention should be paid to disparities in K values between corneal vertex and pupil center. In cases of significant K value differences, preoperative adjustments and thorough patient communication are recommended. Exploring the underlying nature of these anomalies is essential to unravel the mystery of these ‘refractive accidents’,” emphasized Dr. Luo.
Optimizing visual outcomes in corneal refractive surgery
Meanwhile, Dr. Zhang Fengju (Beijing Tongren Hospital, Capital Medical University, China) suggested several key points to further enhance the visual quality of corneal refractive surgery.
“Firstly, meticulous and rational screening of candidates is essential to ensure optimal outcomes. Secondly, it is crucial to tailor surgical plans to each patient’s unique conditions,” said Dr. Zhang.
Additionally, she highlighted the importance of minimizing the biomechanical impact on corneal tissue stability to the greatest extent possible. Preserving corneal biomechanics is crucial for maintaining the structural integrity of the eye and ensuring optimal visual outcomes.
Also, postoperative education and care are emphasized as particularly vital aspects. Furthermore, the use of clean diagnostic and treatment facilities along with precise surgical techniques are identified as critical factors in improving visual quality.
Last but not least, Dr. Zhang highlighted the importance of preventing visual damage post-surgery in cases of high myopia, in order to ensure lifelong eye health. These strategies collectively contribute to advancing the effectiveness and safety of corneal refractive surgery while prioritizing patients’ visual well-being.
OCT’s vital role in phakic IOL implantation
To end the session, Dr. Han Wei (Second Affiliated Hospital, Zhejiang University School of Medicine,China) discussed the crucial role of anterior segment optical coherence tomography (OCT) in phakic IOL (Implantable Collamer Lens [ICL] or Toric Implantable Collamer Lens [TICL]) implantation surgery.
He emphasized the importance of adhering to standardized surgical techniques to ensure patient safety when performing phakic IOL implantation, and underscored the need for every step of the operation to be meticulously executed with precision and strict adherence to protocol. “While speed is desirable, safety remains paramount during the surgery. Ultimately, we should focus on protecting the patient’s crystalline lens,” he explained.
Dr. Han also highlighted the significance of real-time vault measurement assessment during surgery in enhancing the accuracy of ICL implantation. This is where OCT plays a crucial role.
Emphasizing the significant clinical and research value of anterior segment OCT during Phakic IOL procedures, Dr. Han said that this imaging technique aids in precise incision and intraocular lens positioning. It enhances assessment accuracy and provides valuable insights into anterior segment tissue anatomy and surgical processes. “The real-time information provided by the anterior segment OCT also serves as a crucial tool for surgical judgment and decision-making during ICL implantation procedures,” he noted.
Editor’s Note: Reporting for this event took place during the 36th Annual Meeting of the Asia-Pacific Association of Cataract and Refractive Surgeons (APACRS 2024), held from May 30 to June 1, 2024 in Chengdu, China. The 36th APACRS annual meeting is jointly organized with the 24th CSCRS (Chinese Society of Cataract & Refractive Surgery) annual meeting.