A new topography-guided laser vision correction system is set to redefine refractive surgery
Laser vision correction has long aimed for spectacle independence, but true satisfaction extends beyond mere sharpness. A new era dawns with topography-guided treatments, addressing both low- and high-order aberrations for optimal visual quality. OCTAVIUS, a CE-marked system, offers customizable ablation profiles, bringing surgeons closer to achieving complete patient contentment.
Laser vision correction is among the most commonly performed surgeries in the world,¹ which makes it imperative for surgeons to continue striving for greater safety and efficacy.
The laser corneal ablation procedure has undergone several refinements since its introduction.² Early ablation profiles were plagued with deficiencies in laser design and delivery that induced higher-order aberrations (HOAs) and caused visual disturbances postoperatively.
The current standard for laser vision correction is wavefront-optimized treatment, which utilizes population-based ablation profiles to maintain a prolate corneal shape, thereby decreasing treatment-induced HOAs.
However, wavefront-optimized ablation only treats lower-order aberrations (spherical and cylindrical errors) without correcting preexisting HOAs.² Uncorrected HOAs can degrade visual quality—especially in dim light—by reducing image contrast and sharpness,³ and producing optical phenomena like glares and halos.
This can lead to a ’20/20 unhappy’ patient who is dissatisfied with their postoperative visual outcome despite 20/20 vision, due to a deterioration in optical quality.
Beyond 20/20 vision
To correct preexisting HOAs, ablation profiles need to be tailored to each patient’s preoperative corneal or ocular aberrations. The advent of wavefront-guided treatment introduced the concept of individualized corneal ablations, with treatment profiles based on patients’ unique ocular aberrometry measurements that corrected both low- and high-order aberrations while inducing minimal HOAs.²
Although a wavefront-guided approach has theoretical advantages over wavefront-optimized treatment, real-life outcomes with both techniques have not been radically different.²
While wavefront-guided ablation induced significantly lesser HOAs in eyes with preoperative root-mean-square (RMS) HOAs > 0.3 µm, no statistically significant differences were noted in eyes without considerable preoperative HOAs (RMS HOAs < 0.3 µm).⁴
This can be attributed to less precise ablation resulting from the inherent variability of wavefront aberration measurements, which are influenced by factors such as tear film distribution, accommodation state, pupil size and pupil center shifts.⁵⁻⁷ Aberrometry measurements are also difficult to acquire in eyes with highly irregular corneas or media opacities.
Wavefront vs. topography
Compared to wavefront-guided treatment that corrects total ocular aberrations, topography-guided ablation solely corrects corneal aberrations, smoothening corneal irregularities to fit an ideal curve centered around the corneal vertex. This makes topography-guided ablation highly repeatable and predictable, as measurements are not pupil-dependent and are unaffected by accommodation or intraocular aberrations.⁸
Accuracy is further increased by analyzing more points on the cornea and treating more peripheral aberrations compared to wavefront-guided ablation.⁸ Topography-guided ablation is also effective in eyes with significant aberrations or corneal opacities, such as eyes with keratoconus, postsurgical corneal ectasias or traumatic corneal scars.
In previous studies, topography-guided treatment has been observed to achieve predictable outcomes and improve visual symptoms,⁹ with significantly lesser HOAs induced compared to wavefront-optimized treatment.¹⁰
OCTAVIUS—A new frontier in laser correction

The OCTAVIUS Customized Corneal Treatment, recently CE-marked and introduced to the TENEO™ 317 Model 2 excimer laser platform (Bausch & Lomb Technolas, Munich, Germany) [Figure 1], represents a leap forward in the optimization of laser vision correction.
OCTAVIUS allows surgeons to customize treatment via two topography-guided ablation strategies: (a) OCTAVIUS CT anterior, based on anterior corneal topography, and (b) OCTAVIUS CT total, based on the total (anterior + posterior) corneal topography. The CT total strategy is particularly useful in eyes with discrepancies in anterior and posterior corneal surface profiles, as incorporating the contribution of posterior corneal astigmatism can increase treatment accuracy.¹¹
OCTAVIUS offers further treatment customization by allowing surgeons to adjust the intensity of ablation on a sliding scale from 0% to 100%, making it a uniquely tissue-preserving procedure that can be especially valuable in eyes with limited corneal stroma post-refractive surgery.
Real-world results with OCTAVIUS
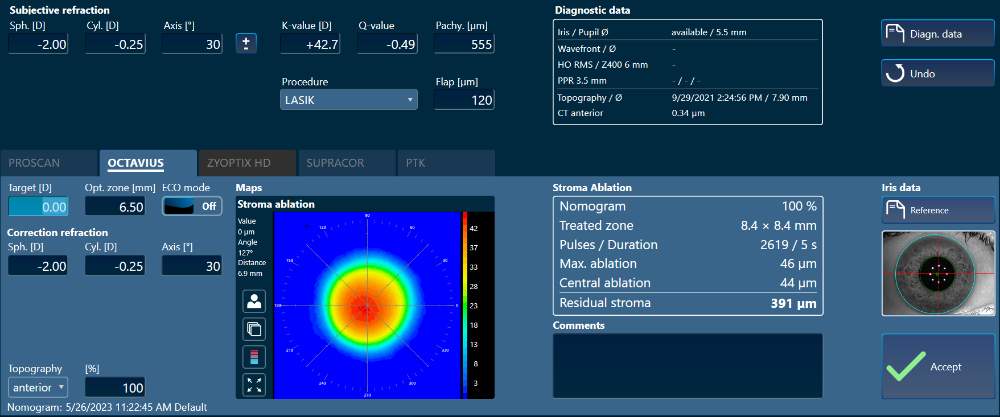
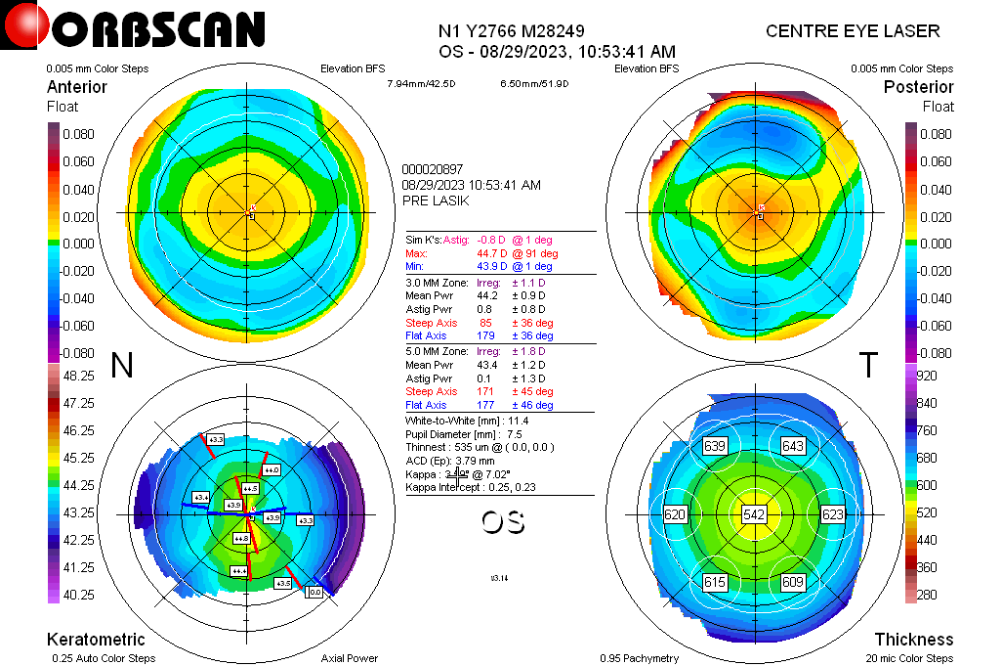
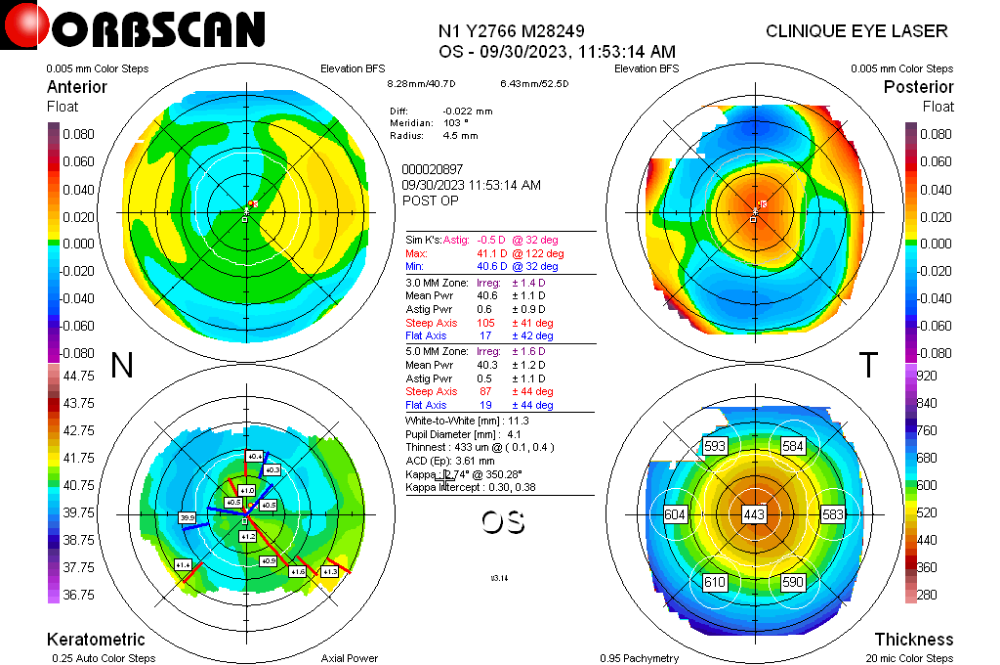
I had the opportunity to perform corneal ablations with OCTAVIUS at my clinical practice in Sousse, Tunisia. Corneal treatments were easy to perform without the need for complex calculations, as ablation profiles were customized by the software by integrating the manifest refraction and the unique topographic data measured for each patient [Figure 2]. The results were presented at the 42nd Annual Congress of the European Society of Cataract and Refractive Surgeons (ESCRS),12 and briefly recapitulated here.
Visual and refractive outcomes were studied in 60 eyes of 39 patients (21 bilateral, 18 unilateral) treated with OCTAVIUS CT anterior strategy with 100% ablation intensity.
Patients were followed up for one-month post-procedure. Although topography-guided ablation is most useful in highly aberrated eyes, I decided to include all patients, regardless of corneal aberrations, to study the utility of this technology in a population similar to that likely to be encountered in routine practice.
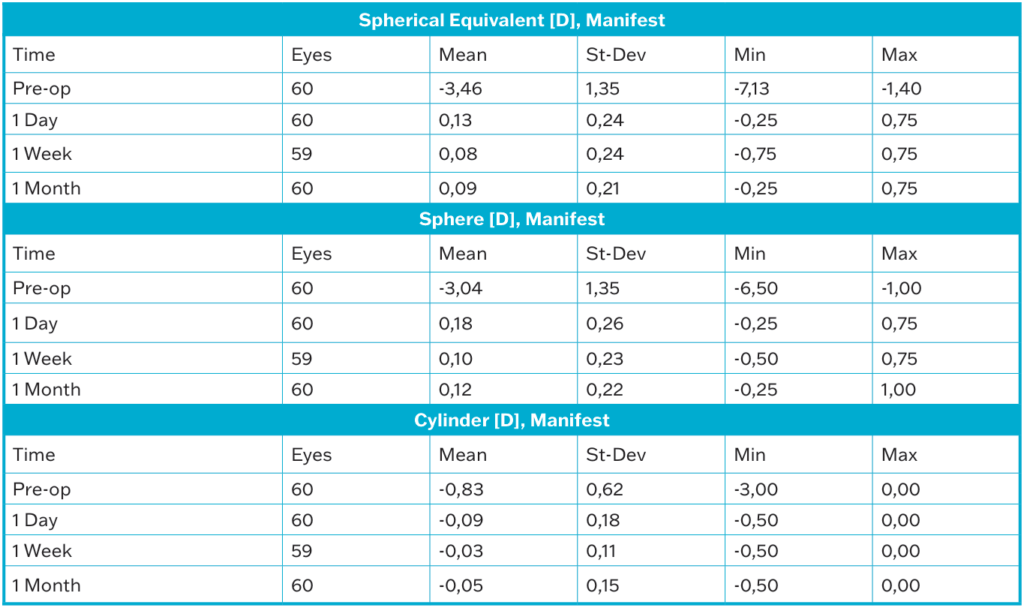
One month postoperatively, mean manifest spherical equivalent (SE) reduced from -3.46±1.35 D at baseline to 0.09±0.21 D, while manifest cylinder reduced from -0.83±0.62 D to -0.05±0.15 D [Table 1].
Binocular uncorrected distance visual acuity (UDVA) of 20/20 or better was achieved in 100% eyes; 86% achieved UDVA of 20/16 or better (compared to 5% with corrected distance visual acuity (CDVA) of 20/16 or better at baseline), and 24% eyes achieved UDVA of 20/12.5 or better (compared to zero eyes with CDVA of 20/12.5 or better at baseline). So, with OCTAVIUS, most patients achieved better uncorrected binocular vision than their best spectacle-corrected preoperative vision.
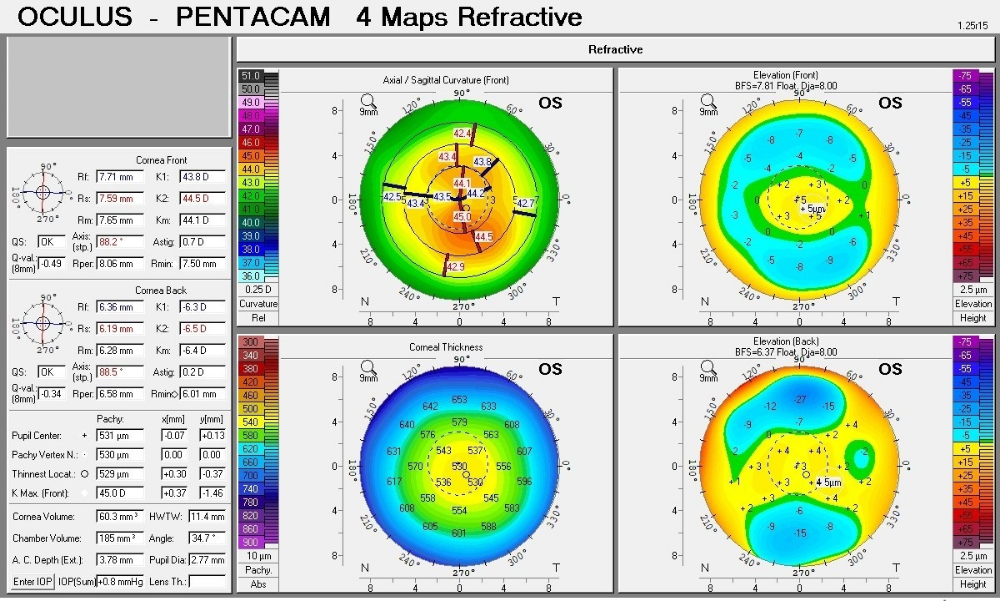
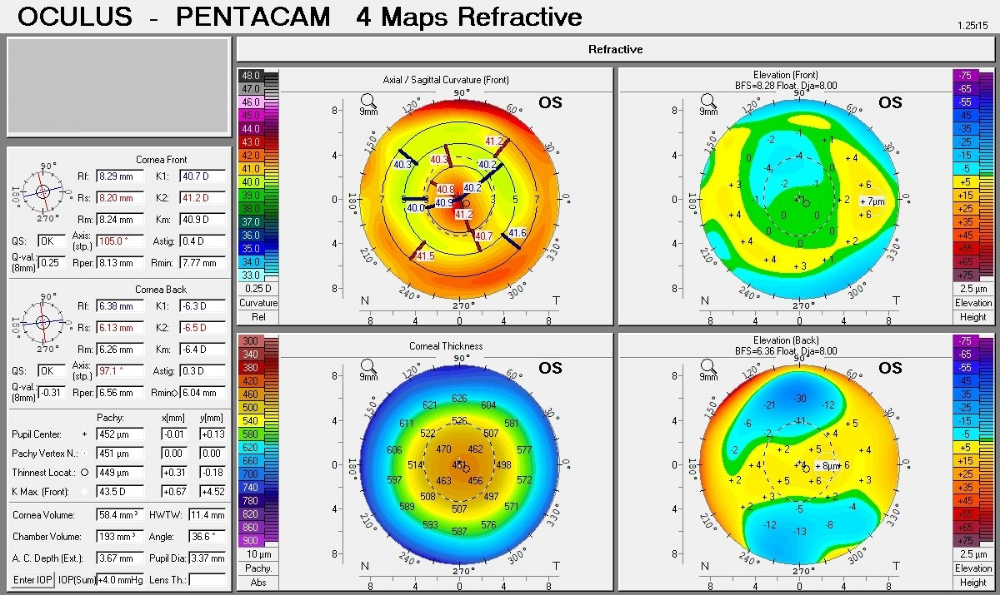
The procedure also showed high predictability with 98.3% of eyes within ±0.5 D of their intended postoperative SE and 62% being within ±0.13 D. Immediate refractive improvements were observed on the first postoperative day (mean SE: 0.13±0.24), stabilizing by one week (mean SE: 0.08±0.24) and remaining stable at one month of follow up (mean SE: 0.09±0.21). OCTAVIUS also showed high safety, with no eyes showing loss of one or more lines of CDVA. A gain of one and two lines of binocular CDVA was seen in 57% and 43% eyes, respectively. Improvements in CDVA could be attributed to the correction of corneal aberrations by OCTAVIUS [Figures 3 and 4].
Patient satisfaction and visual quality
Beyond the quantitative visual acuity gains, what I found most gratifying was the overwhelmingly positive response from my patients regarding their quality of vision. Patients were highly satisfied and reported seeing better without glasses postoperatively than they could with glasses preoperatively, and most patients reported improvements in night vision with reduction in halos. It was clear that the customized topography-guided ablation by OCTAVIUS had not only preserved visual quality, but actually improved it.
These outcomes are in line with those reported for topography-guided ablations in the literature.⁸ Although further studies will be required to establish the safety and efficacy of OCTAVIUS, the sound treatment principle and uniquely customizable strategies make it likely that OCTAVIUS will improve visual outcomes in a wide range of refractive conditions.
Supranormal vision and beyond
Corneal ablation with OCTAVIUS achieves predictable and stable outcomes with high efficacy and safety, making it a promising new tool in the refractive surgeon’s armamentarium. Its highly customizable topography-guided ablation profiles may bring surgeons closer to reaching the ultimate goal of refractive surgery: Supranormal uncorrected visual acuity and optical quality, leading to complete patient satisfaction.
Editor’s Note: A version of this article was first published on CAKE Issue 25.
Contributor
Dr. Fathi Nouira is a cataract and refractive surgeon at Clinique Ophtalmologique de Laser Excimer, Sousse, Tunisia.
References
- Sandoval HP, Donnenfeld ED, Kohnen T, et al. Modern laser in situ keratomileusis outcomes. J Cataract Refract Surg. 2016;42(8):1224 -1234.
- Stonecipher K, Parrish J, Stonecipher M. Comparing wavefront-optimized, wavefront-guided and topography-guided laser vision correction. Curr Opin Ophthalmol. 2018;29(4):277-285.
- Williams D, Yoon GY, Porter J, et al. Visual Benefit of Correcting Higher Order Aberrations of the Eye. J Refract Surg. 2000;16(5):S554-9.
- Feng Y, Yu J, Wang Q. Meta-Analysis of Wavefront-Guided vs. Wavefront-Optimized LASIK for Myopia. Optom Vis Sci. 2011;88(12):1463-1469.
- Maeda N. Clinical applications of wavefront aberrometry – a review. Clin Exp Ophthalmol. 2009;37(1):118-129.
- Dobos MJ, Twa MD, Bullimore MA. An evaluation of the Bausch & Lomb Zywave aberrometer. Clin Exp Optom. 2009;92(3):238-245.
- Atchison DA, Mathur A. Effects of Pupil Center Shift on Ocular Aberrations. Invest Ophthalmol Vis Sci. 2014;55(9):5862-5870.
- Ramamurthy S, Soundarya B, Sachdev G. Topography-guided treatment in regular and irregular corneas. Indian J Ophthalmol. 2020;68(12):2699-2704.
- Stulting DR, Fant BS. Results of topography-guided laser in situ keratomileusis custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg. 2016;42(1):11-18.
- Cheng SM, Tu RX, Li X, et al. Topography-Guided Versus Wavefront-Optimized LASIK for Myopia With and Without Astigmatism: A Meta-analysis. J Refract Surg. 2021;37(10):707-714.
- Zhou W, Stojanovic A, Utheim TP. Assessment of refractive astigmatism and simulated therapeutic refractive surgery strategies in coma-like-aberrations-dominant corneal optics. Eye Vis (Lond). 2016;3(1):13.
- Nouira F. First Experience With Topography Guided Ablation Treatment Based On OCT Readings. Poster presented at the Annual Congress of the European Society of Cataract and Refractive Surgeons; September 6-10, 2024; Barcelona, Spain.