Ophthalmology gets political, poetic and polygenic…AAO 2025’s opener hit all the right notes (and nerves).
Ophthalmology’s sharpest vision doesn’t always come from a microscope. Sometimes, it comes from a microphone.
From policy punches and AI pilots to a soulful violin solo, the Opening Session on Day 2 of the American Academy of Ophthalmology Annual Meeting 2025 (AAO 2025) had it all: advocacy with attitude, data with drama and a few gentle reminders that the fight for sight is as human as it is high-tech.
A call for advocacy
If ophthalmology had a secret weapon, it wouldn’t be a femtosecond laser. It’d be good, old-fashioned advocacy.
Outgoing Academy President Dr. Michael Repka (USA) kicked things off with a rallying cry for getting loud, getting involved and maybe getting a little political.
“Healthcare advocacy remains key to our mission,” Dr. Repka told attendees. “As a medical specialty society, we must remain engaged with whomever is in leadership to protect our patients and advocate for our healthcare priorities.”
And there’s plenty to fight for. The math on Medicare payments? It doesn’t add up. “Practice cost inflation has been nearly 60% over two decades, while reimbursements have increased just 6%,” he pointed out, a sobering stat that landed with a collective sigh.

Then there’s the dreaded PA—no, not physician assistant, the other one. “Prior authorization is reported by 93% of physician groups to delay or deny necessary care, yet the decision is overturned 82% of the time on appeal,” Dr. Repka said, suggesting that bureaucracy may be the only thing growing faster than inflation.
He also sounded the alarm for the National Eye Institute (NEI), which could face budget cuts or restructuring. “The NEI has an exceptional record of accomplishment, but that has not stopped the Congress—while looking for cost savings—to consider collapsing the NEI into a new brain institute,” he cautioned.
His advice? Stop watching from the bleachers. “Get involved locally, nationally or, perhaps better, both,” he urged.
EyeCare America levels up
Next on the docket: a glow-up for EyeCare America, the Academy’s beloved public service program, which turns 40 this year and is aging far better than most health policies.
“EyeCare America was established as the first independent public eye health program with national reach,” explained Academy CEO Dr. Stephen McLeod (USA). “To date, EyeCare America has connected approximately 10,000 volunteer physicians with more than 150,000 patients in need of eye care.”

But after four decades of serving mainly seniors, the program is ready for its next act. “There are millions across America under 65 who are uninsured or underinsured, but who do need access to health care, including eye care,” said Dr. McLeod.
READ MORE: Pearls Under Pressure: Practical Glaucoma Tips from AAO 2025
The Academy has its sights set on federally qualified health centers (FQHCs)—a massive network serving 30 million Americans. “Two-thirds of these patients are at or below 100% of the federal poverty guideline,” he noted, “and 20% of these patients were completely uninsured.”
The kicker? “Only about a third of these health centers provide any vision services on-site,” he said.
His solution is refreshingly simple: expand EyeCare America to cover everyone aged 18 and up who hasn’t seen an ophthalmologist in the past three years. No insurance, no problem.

Speaking of serving the underserved, Professor Hugh R. Taylor, AC, MD, FRANZCO, recipient of the 2025 AAO Laureate Recognition Award, has built a distinguished career focused on preventing blindness in vulnerable communities—from Australian Aboriginal populations to those in developing regions worldwide. His groundbreaking efforts in research and advocacy have played a pivotal role in combating trachoma and onchocerciasis.
A case for AI
To drive this new phase forward, the Academy is turning to its new favorite resident—artificial intelligence. Dr. McLeod shared results from a pilot program at Delaware’s Henrietta Johnson Medical Center, where AI-powered diabetic retinopathy screening has been quietly changing lives.
“More than 500 patients were screened over 18 months,” he said. “More than a third of the gradable images had referable diabetic retinopathy. About 60% of these actually had vision-threatening findings.
And with disease detection, AI found opportunity. The project connected at-risk patients to EyeCare America’s volunteer network faster than any manual referral process could.
Plus, thanks to some chivalrous funding, the expansion just got turbocharged. “This year, the Knights Templar Foundation granted the Foundation of the American Academy of Ophthalmology $1,500,000 to support this initiative, thereby facilitating the largest expansion of the EyeCare America program since its inception,” Dr. McLeod announced.
The great call conundrum
Incoming Academy President Dr. Christopher Rapuano (USA) then tackled two thorny issues that seem to keep ophthalmologists up at night: who’s covering the ER, and who’s creeping into the surgical suite.
“Over the past 20 years or so, fewer and fewer ophthalmologists around the country—and for that matter around the world—have been willing to take ER calls,” Dr. Rapuano said, citing the rise of ambulatory surgery centers, lack of reimbursement and fading emergency skills.
And guess who’s volunteering to fill the gap? “I can’t believe who wants to be on call,” he said. “Optometrists.”

The situation, he warned, makes scope-of-practice battles “infinitely harder.” But the Academy isn’t sitting idle. It’s planning new trauma and on-call training programs to help ophthalmologists regain confidence (and maybe a little swagger) in emergency settings.
“I would want my family members to be taken care of by an ophthalmologist when they go to an ER with an eye emergency,” he said. “We’re going to try and make that easier.”
Glaucoma gets personal
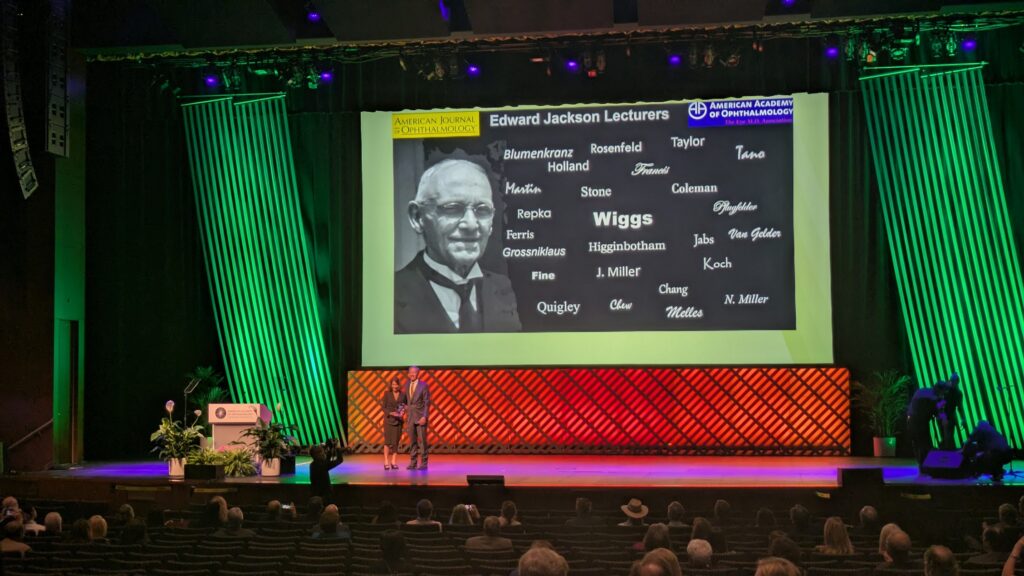
Science fiction officially became science fact during the Jackson Memorial Lecture, delivered by Dr. Janey Wiggs (USA) of Harvard Medical School. Her topic: using genetics to predict glaucoma risk…decades before vision loss sets in.
“DNA testing is a one-time test,” she explained. “It doesn’t change over a lifetime, and people could learn of their high genetic risk years before the disease becomes manifest.”
Her research has pinpointed 12 genes for childhood glaucoma and hundreds more for primary open-angle glaucoma (POAG). By calculating polygenic risk scores (PRS), clinicians could soon identify high-risk individuals and step in early.
She shared the case of a 66-year-old patient who discovered his glaucoma far too late. “His visual field testing showed that he already had advanced glaucoma,” she said. “After genetic testing, we determined that his polygenic risk score was in the 99th percentile.”
Then came the haunting takeaway. “If we could have measured his polygenic risk score 30 years ago, he would have known his risk,” she concluded. “Perhaps before his intraocular pressure increased, he could have had earlier treatment, and his vision may have been preserved.”
A celebration of art and medicine
The session closed on a melodic high note with the Michael F. Marmor Lecture in Ophthalmology and the Arts, featuring world-renowned violinist Rachel Barton Pine (USA). Her performance—complete with Bach’s fugue and a special spin on Beethoven’s Eyeglasses Duet—was the perfect reminder that sight and art share the same rhythm.
“Musicians have an unusual eye challenge,” Ms. Pine said, tying it all together. “When we go to the optometrist, they want to check near vision and distance vision, and neither of those is quite right for sheet music distance.”

Ms. Pine also dropped a cautionary historical note about 18th-century eye surgeon John Taylor, who operated on both Bach and Handel—with tragic results. “It’s not a coincidence that both of them died shortly after their eye operations,” she said, earning a mix of laughter and grimaces from the audience.
READ MORE: Subspecialty Day at AAO 2025: Lenticules, Award Lectures and New Technology in Focus
The takeaway
From battling bureaucracy to decoding DNA, the Academy’s leaders made it clear that preserving sight means more than performing surgery. It means shaping the systems, science and stories that surround it.
And as Ms. Pine’s final notes echoed through the hall, it felt fitting. A perfect encore for a specialty that continues to find harmony between art, advocacy and innovation.
Editor’s Note: The American Academy of Ophthalmology Annual Meeting 2025 (AAO 2025) is being held on 17-20 October 2025, in Orlando, Florida. Reporting for this story took place during the event. This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
