When tea tree oil and cleansers fall short, shine a light on stubborn Demodex blepharitis.
A new study offers a glimmer of light—literally—for eye care professionals managing stubborn Demodex blepharitis (DB). Researchers in the United Kingdom have found that combining intense pulsed light (IPL and low-level light therapy (LLLT) using blue and red wavelengths significantly improved both signs and symptoms in patients unresponsive to standard treatments.
Published in Clinical Ophthalmology, the retrospective study reported notable reductions in eyelid debris, redness and ocular-surface discomfort, all without treatment-related adverse effects.*
The study at a glance
The review included 17 patients (34 eyes), aged 48 to 83 years, all with recalcitrant DB unresponsive to first-line therapies such as tea tree oil or hypochlorous acid cleansers. Participants underwent dual-light treatment using the Eye-light device (Espansione Group; Bologna, Italy) between June 2020 and October 2023.*
Follow-up assessments occurred approximately six months after the final session. Measurements included slit-lamp exams, MYAH (Topcon; Tokyo, Japan) readings and symptom questionnaires such as the Dry Eye Questionnaire-5 (DEQ-5).*
READ MORE: XDEMVY vs. Tea Tree Oil: A closer look at Demodex blepharitis solutions
The results
After treatment, patients demonstrated statistically significant improvements:*
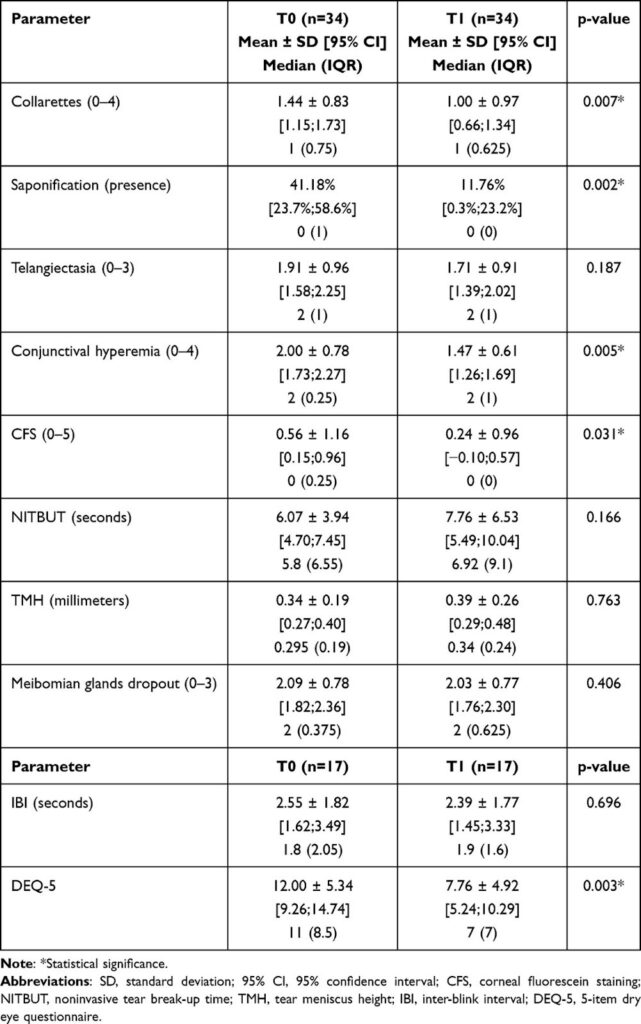
Means, Standard Deviations and 95% Confidence Intervals of Data Collected at Baseline (T0) and After Treatment at the Last Follow-Up Visit (T1)*
- Eyelash debris (collarettes): Decreased from an average score of 1.44 to 1.00
- Foamy secretions (saponification): Reduced from 41.18% to 11.76%
- Redness (conjunctival hyperemia): Improved from 2.00 to 1.47
- Corneal staining: Dropped from 0.56 to 0.24
- DEQ-5 scores: Fell from 12.00 to 7.76
At follow-up, 64.7% of eyes showed at least a one-grade reduction in Demodex presence, and 17.6% achieved complete mite eradication. Importantly, no adverse effects were reported.*
While some measures—such as tear meniscus height (TMH) and non-invasive tear break-up time (NITBUT)—showed non-significant increases, overall ocular-surface health and comfort improved notably.*
Why it matters
Demodex blepharitis accounts for more than 60% of all blepharitis cases and is often linked to dry eye disease (DED) and meibomian gland dysfunction (MGD). Despite a crowded field of treatments—from tea tree oil and ivermectin—consistent success remains elusive due to irritation risks and poor compliance.*
READ MORE: Eyelid Margin Health Series
The authors acknowledged the recent U.S. Food and Drug Administration (FDA) of lotilaner ophthalmic solution 0.25% (Tarsus Pharmaceuticals; California, USA), which has shown “high efficacy in Demodex mites and collarette eradication as well as erythema reduction.” However, they noted that its global availability and impact on broader ocular surface symptoms are still limited.*
Given these gaps, the team explored light therapy as a non-pharmacologic approach targeting both mite load and inflammation simultaneously.*
Eyelid Margin Health Series: Innovative Treatments for Demodex Blepharitis & MGD
How the dual-light therapy works
Patients received IPL in Optimal Power Energy (OPE) mode with wavelengths between 600 to 1200 nm and energy levels of 4.5 to 8.2 J/cm², applied as five flashes along the lower eyelid and lateral canthus. This was followed by LLLT sessions using blue (465 ±40 nm) and red (625 ±40 nm) light for 12 minutes, each via a mask with eyes closed.*
The authors suggest the combined mechanisms—IPL’s photothermal reduction of Demodex and LLLT’s bio-stimulatory and anti-inflammatory effects—may explain the wide-ranging improvements. Notably, previous LLLT studies focused on red light alone, while the addition of blue light here introduces antibacterial and microbiome-stabilizing benefits.*
READ MORE: Espansione’s Blue LM® LLLT on Demodex Blepharitis, Saponification and the Ocular Microbiome
Strengths and limitations
While results were encouraging, the authors cautioned that the study’s retrospective design, lack of randomization or control group and small sample size limit generalizability. Diagnosis was based solely on clinical observation of collarettes without microscopic confirmation. Timing variations in follow-up may also have influenced eradication rates.*
Still, the authors concluded that “combined light therapy with IPL and LLLT employing both blue and red lights seems an effective treatment strategy for patients with recalcitrant Demodex-associated blepharitis to reduce collarettes score and saponification while also improving main ocular surface parameters and patients’ symptoms.”*
The takeaway
For eye care professionals wrestling with mites that refuse to quit, the combination of IPL and blue-red LLLT may offer a practical, well-tolerated solution, no daily scrubbing or stinging lids required.
While pharmacologic innovation like lotilaner continues to evolve, this study shines light on a promising clinic-based, drug-free alternative for DB management.
***Farrant S, Giannaccare G, Lim CHL, et al. Intense pulsed light combined with low level blue and red light therapy for Demodex-associated blepharitis. Clin Ophthalmol. 2025;19:2575-2585. .
Editor’s Note: This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
