Most often, the topic of intraocular lenses (or IOLs) arises when discussing cataract surgery. After all, it’s during this procedure that the clouded lens is replaced by a new, artificial one. However today, surgeons also have a new batch of patients looking for clear vision: those with presbyopia.
When IOLs were first introduced, the monofocal was king. Now considered a basic or standard IOL, this lens gives good distance vision but lacks in intermediate and near — and as a result, leaves patients in spectacles, postoperatively. As patients demanded better outcomes — and clearer vision at all distances — premium IOLs, like trifocals and multifocals, entered the market. But unfortunately, these IOLs still struggle to deliver spectacle-free vision at all distances; they can also be plagued by photic phenomena like glare and halos.1
The Unmet Need in Presbyopia Correction
Lack of vision at all distances coupled with photic phenomena has created a clear unmet need in presbyopia correction — and one that SIFI, an Italian group of companies focusing on R&D, manufacturing, and commercialization of ophthalmic products, is addressing through its one-of-a-kind WELL Fusion optical system. This system utilizes two bilaterally implanted EDOF IOLs, the Mini WELL and Mini WELL PROXA, to provide clear, spectacle-free vision at all distances with negligible photic phenomena and minimal to no loss of contrast sensitivity.
Using the same non-diffractive extended depth of focus (EDOF) platform and with wavefront-engineered complementary IOL design, both quantity and quality of vision are improved with WELL Fusion.
In this system, extended depth of focus is created by inducing targeted amounts of spherical aberration in the concentric optical zones in the central part of the IOLs. This creates one continuous focus — without dividing the light beam — resulting in a lower risk of photic phenomena compared to other multifocal IOLs. That means with WELL Fusion, patients can achieve uninterrupted vision across all distances without compromise, including excellent near vision and stable and consistent visual performance up to -3.5 D defocus.2
Clinical Experience and Results
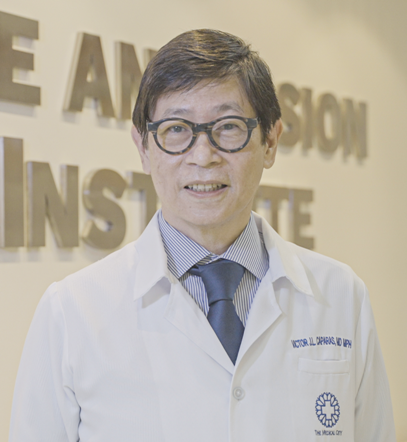
Recognizing the capabilities of this new system is Dr. Victor Caparas, an ophthalmologist in Manila, Philippines. He has been studying and implanting the SIFI family of IOLs for the past six years, including the Mini WELL (from 2017), the Mini WELL Toric (from mid-2018), and the Mini WELL PROXA (from late 2020).
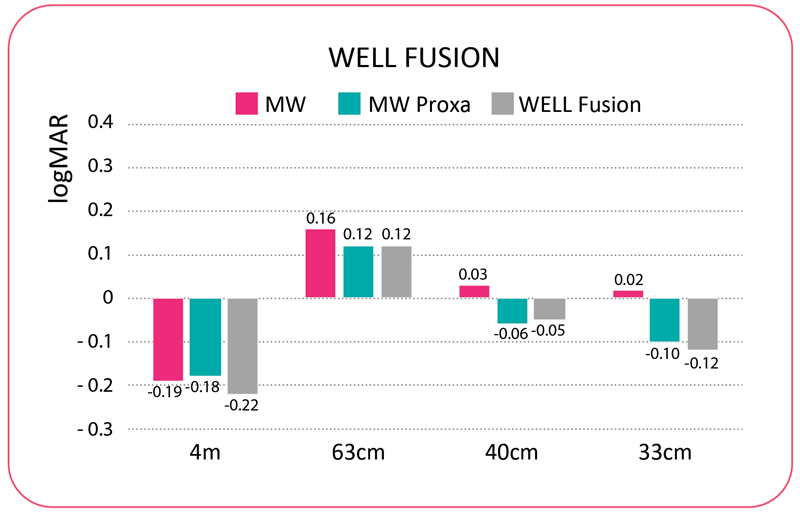
As a whole, Dr. Caparas reported similar and good visual results, with patients reporting high satisfaction with these three IOLs. For quantity of vision, binocular distance (4 m) was better than -0.1 logMAR; intermediate (63 cm) was 0.1 to 0.2 logMAR; and near (40 cm) ranged from 0.0 to 0.2 logMAR. Further, with WELL Fusion (and the Mini WELL PROXA) near vision at 33 cm was better than -0.1. For quality of binocular vision, Dr. Caparas said that all of the studied IOLs show similar, extremely low halo and glare with logCS (contrast sensitivity) ranging from 1.67 to 1.82, which is closer to monofocal contrast sensitivity than a diffractive multifocal.
Similar results for the EDOF Mini WELL were reported by Auffarth et al., in 2020: Mean UDVA was -0.01 ± 0.15; UIVA was 0.03 ± 0.10, and UNVA was 0.10 ± 0.11 logMAR. Further, he reported a mean halo size of 33.06 ± 14.25, mean halo intensity of 38.00 ± 18.51, mean glare size of 23.85 ± 10.43, and mean glare intensity of 42.23 ± 13.22.3 They concluded that the Mini WELL “provides good visual acuity across various distances and functional reading ability provided at a near range, and delivers an enhanced contrast sensitivity while causing a low incidence of photic phenomena.”
In October 2020, Dr. Caparas began his study of WELL Fusion with 40 eyes of 20 patients. They were followed for 90-105 days; 19 patients completed their postoperative visits. In this clinical study, Dr. Caparas evaluated the visual function, quality of vision, subjective outcomes, and safety after implantation with Mini WELL and Mini WELL PROXA. This was a part of a multicenter, observational, prospective, single-arm, and investigator-driven study with visual function and quality evaluated at 3 months following the second eye implantation.
To illustrate how WELL Fusion goes a step above competing IOL platforms, Dr. Caparas shared some of his postoperative data: Regarding quantity of vision, distance VA (4 m) was -0.22 logMAR; intermediate VA (63 cm) was 0.1 logMAR; near VA (40 cm) was -0.05 logMAR; and near VA (33 cm) was -0.12 logMAR. Snellen results showed the following: distance VA of 20/12; intermediate VA of 20/25; near (40 cm) VA of 20/18; and near (33 cm) VA of 20/15.
“[With WELL Fusion,] the results have been great. Now, we have patients that can read up to 30-35 cm as opposed to the first Mini WELL studies,” he shared. Further, thanks to its wider depth of focus, gaps in near vision are filled. “The Mini WELL gives us good far and intermediate vision,” said Dr. Caparas. “On the other hand, the Mini WELL PROXA gives us excellent near vision. Together, these [IOLs] give us an uninterrupted range of vision from infinity to all the way to about 30-35 cm.”
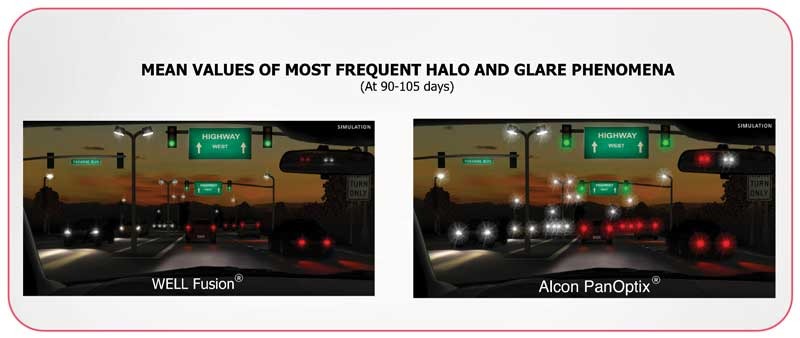
Further, when assessing quality of vision, using the Halo and Glare Simulator software, Dr. Caparas found extremely low glare and haloes: halo size (20); halo intensity (28); glare size (15) and glare intensity (17). Meanwhile, he reported contrast sensitivity at 40 cm was 1.82 (logCS).
With such impressive data, it’s clear that SIFI’s focus on improving both quantity and quality of vision is resulting in improved outcomes. “WELL Fusion fulfills the need for excellent visual acuity at all distances: far, intermediate, near, and very near. Just as important, it affords this without the disabling photic phenomena that very often, for the patient, negates the good results in visual acuity,” said Dr. Caparas.
“This offers patients more functionality, more spectacle independence, and less light dependence,” he continued. “For doctors, this means less complicated options can be presented to patients — for example, no mix-and-match or micro-monovision options — and it provides reliability in both visual acuity and near absence of photic phenomena,” he said. “All of this equates to happier, more satisfied patients.”
The ‘Right’ IOL in the ‘Right’ Patient
Before implanting a premium IOL, surgeons must consider numerous elements — from anatomic to lifestyle — to achieve the best possible visual outcome. Surgeons must obtain exact measurements, understand the IOL’s characteristics, and discuss the patients’ demands and lifestyle.
For example, the patient’s age and activity level should be considered, as well as their occupation and lifestyle needs. “It’s important to understand the needs and preferences of the patient: Does the patient have reasonable demands? Do they drive at night? Do they read or use laptops or smartphones often? Do they prefer distance vision over near, or vice versa? These all must be considered,” said Dr. Caparas.
Other factors include:
• Spectacle tolerance: Does the patient understand the possibility of spectacle use for prolonged, visually- demanding tasks?
• Personal motivation: Do they understand the need for neuroadaptation and can they wait for visual outcomes to improve?
• Psychological health: Are there any mental health issues?
• Eye status: Do they have dry eye, refractive error, cataract, or any posterior segment pathology?
And although these are all key considerations when choosing an IOL, Dr. Caparas shared that some of these factors are not as critical with WELL Fusion — and that’s because the optical system allows the patient profile to be extended, thanks to a full range of focus from far through near along with a very high quality of vision.
“Any patient who desires both good distance and near vision, and understands the need for adaptation will be an ideal candidate for WELL Fusion,” continued Dr. Caparas. “This is based on the visual results, absence of photic phenomena, good contrast sensitivity, — and because WELL Fusion provides the whole range of very good to excellent vision, with excellent quality.”
Pre-op: Measure and Counsel
Preoperatively counseling patients can help improve postoperative outcomes: Patients who know what to expect will generally be happier. Dr. Caparas shared that before proceeding with WELL Fusion, he counsels patients on the effects dry eye could have, as well as the time required for neuroadaptation (albeit it rapid).
Dr. Caparas then described some of his preoperative processes with WELL Fusion. For example, he checks for eye dominance, dry eye status, and pupil status. He reviews the biometry to ensure a good quality scan and that the patient has normal K values (40 to 47 D) and astigmatism of less than 0.75 D.
Using the Pentacam AXL-Wave (Oculus Optikgeräte GmbH, Wetzlar, Germany), he shared patients should be within the following ranges: chord mu of <0.4 mm (surrogate for angle kappa); spherical aberration/Z40 (6.0 mm) of <0.3-0.5 µm; HOA (4.0 mm) of <0.3-0.5 µm; and Q value/asphericity should be negative (prolate cornea).
Meanwhile for aberrometry, Dr. Caparas uses the iTrace (Tracey Technologies, Houston, Texas, USA). He noted that patients should be within angle alpha (limbal center and visual axis) of <0.5 mm; and angle kappa (pupil center and visual axis) of <0.5 mm. He also measures the corneal, internal, and total eye aberrations using Chang analysis.
Intra-op: Techniques and Considerations
While WELL Fusion may provide revolutionary outcomes, the surgical procedure to implant the IOLs is more traditional. “I use the same technique as with all other of my phacoemulsification surgeries: I make a 2.2 mm temporal incision and a 5.5 mm capsulorhexis, I fill the capsular bag with sodium hyaluronate/HPMC viscoelastic for implantation of the IOL, and then I meticulously polish the capsule and remove the OVD (ophthalmic viscosurgical device).”
Dr. Caparas shared that he follows SIFI recommendations by implanting the Mini WELL in the dominant eye and the Mini WELL PROXA in the non-dominant eye. “I don’t have any experience doing so otherwise [implanting the Mini WELL in the non-dominant eye and vice versa], but I do have extensive experience with monovision using monofocal IOLs, and I’ve hardly seen any difference in using the dominant eye for distance or for near vision,” he said.
Through his experience with WELL Fusion, Dr. Caparas has identified further pearls that allow him to achieve the best results for patients. “We discovered early in our studies that aiming for a slightly hyperopic postoperative refraction resulted in better distance vision and happier patients,” he explained. “So we have adjusted our target, or alternatively, adjusted the recommended A constant.”
He continued: “Also, I avoid very small pupils (<2.0 mm, photopic) as we have observed distance vision to suffer under bright conditions, like driving in very bright daylight.”
In addition, Dr. Caparas shared that dry eye can significantly affect performance, so he recommends managing dry eye and using lubricants early, even before surgery.
Post-op: Show me the Outcomes
Through his study of WELL Fusion, Dr. Caparas reports that patient satisfaction is high following surgery. “All subjects in our study had excellent vision — good enough for them to rate their quality of vision and spectacle independence very highly at three months post-op,” he said. In general, it takes most patients between one and three months to adapt, although some patients may have significant adaptation by one month.
This shows that patients are adapting rapidly — and what’s more, most of them are spectacle-free: “Sixteen of 18 subjects from our WELL Fusion studies are 100 percent spectacle independent (score 1.0 out of 5, where 1 is “never” and 5 is “all the time”). Of the remaining subjects, one scored 1.67, while the other scored 3.0.”
Dr. Caparas shared that the quality of vision questionnaire reported the mean score assessing photic phenomena was 83% (the higher, the better). The mean overall spectacle independence scores (1 is best and 5 is worst) were 1.12 for distance vision; 1.18 for intermediate vision; and 1.18 for near vision.
Further, it’s so uncommon for patients to report haloes or glare with WELL Fusion, that Dr. Caparas said he’s had to describe them to patients. “Often when performing the simulator test, halo and glare have to be explained, as patients report that they have not experienced any — even when driving at night,” he shared.
“This is in contrast to other IOLs, especially diffractive IOLs, where haloes and glare are significant — even after months and years of neuroadaptation and learning to tolerate the dysphotopsia,” continued Dr. Caparas.
Following surgery, very few side effects have been reported, which Dr. Caparas attributes to small pupils and dry eye. “A small number of patients have mentioned decreased distance vision in very bright conditions — we attribute this to very small (<2.0 mm) pupils in photopic conditions,” he explained. “Also, the effects of dry eye are pronounced with this type of IOL, as with other similar lenses.”
But what are the patients actually saying? Survey says they’re happy — with a mean score of 1.06 in the study’s spectacle and light dependence questionnaire (where 1 is best and 5 is the worst). Patients also reported that they would have the same lens implanted again and would recommend the IOLs to a friend (both scores of 1.0). In total, only one patient scored less than a 1.0 in regard to satisfaction at 1.25.
Deliver Results with WELL Fusion
With so many “answers” to presbyopic correction, it’s refreshing to come across a real solution in terms of quantity and quality of vision. Indeed, when compared to other IOLs, WELL Fusion provides excellent VA, range of vision, and visual quality with close to zero photic phenomena.
Another added benefit? “WELL Fusion retains the same excellent visual qualities of the Mini WELL, while achieving even better near vision at 33 cm,” said Dr. Caparas.
It’s clear that WELL Fusion offers numerous benefits to doctors and patients. But perhaps the most poignant takeaway is this: The results and satisfaction with WELL Fusion is changing the face — and expectations — of presbyopia correction.
“My attitude to presbyopia-correcting lenses has changed,” said Dr. Caparas. “I have more confidence in results and their predictability, I have more happy patients, with hardly any complaints. And finally, implantation of premium IOLs has also increased significantly.”
References
- Sieburth R, Chen M. Intraocular lens correction of presbyopia. Taiwan J Ophthalmol. 2019; 9(1): 4–17.
- SIFI. (2021). Clinical Experiences with WELL Fusion [White paper].
- Auffarth GU, Moraru O, Munteanu M, et al. European, Multicenter, Prospective, Non- comparative Clinical Evaluation of an Extended Depth of Focus Intraocular Lens. J Refract Surg. 2020;36(7):426-434.