In Krakow yesterday a local Polish man realized his vision was fading somewhat, perhaps a case of early onset presbyopia, so he decided to visit his local optometrist. Sitting down for his examination, our Polish friend was asked to read the bottom line of the chart containing the following letters; Z, Y, K, W, Z, C, Z, S, R, a routine test of course.
Straining but just about able to make the letters out, he read them aloud as requested. However, as he did so a look of confusion appeared on his face. The optometrist asked “oh so you can read the letters?”
Our Polish friend responded “read them out? I know that guy Zykwzczsr!”

Pan. Zykwzczsr, to ty? Dobrze cię widzieć! (Translation: Mr. Zykwzczsr is that you? Good to see you!)
On behalf of the entire Media MICE team, apologies for forcing this old joke on you, we could not resist the opportunity. Jak się masz? And welcome to Day Two of the European Society of Cataract and Refractive Surgeons (ESCRS) 2021 Winter Meeting, and we promise that was the last joke about Polish spelling. Indeed, the Polish language has some of the hardest pronunciations among Slavic languages but it has a beauty all of its own, much like the ancient city of Krakow where the conference was slated to take place.
Crohn’s and Cornea: A Match Made in Hell
Day two is the only full day session of this year’s ESCRS Winter Meeting and it contained some topics of discussion as complicated and yet enticing as the Polish spelling system. Proceedings kicked off with Cornea Cases, which was organized in conjunction with EuCornea. A number of fascinating case studies were presented with a particular highlight being Relentless Peripheral Ulcerative Keratitis with Corneal Perforation in Crohn’s Disease by Dr. Sara Pereira of the University of Lisbon, Portugal.
The patient was a 32-year-old with a history of severe Crohn’s disease and presented with bilateral peripheral ulcerative keratitis (PUK) with corneal perforation in November 2019. A bilateral amniotic membrane was applied. However, the perforation recurred in February 2020 characterized by progressive melting. Ouch.
A second membrane was applied with a third following in May of the same year. By February 2021 the patient was still experiencing severe corneal thinning and peripheral melting. However, a change to azathioprine had improved the symptoms of extraintestinal manifestations.
Dr. Pereira concluded that the “disposition of circulating immune complexes plays a major role in the development of PUK and that a multidisciplinary approach is essential.” She stated that this was one of the most severe cases of PUK secondary to Crohn’s disease reported. According to the doctor, a corneoscleral crescent transplantation “could be of interest to the patient.”
Like J.J. Abrams we Love Our Lenses
One of two main symposia of the day, Optimizing Your Refractive Outcomes Before Cataract Surgery’s title may not seem as attention grabbing as Crohn’s disease and corneal perforation (which honestly stunned some members of the Media MICE team). However, it was a fascinating and highly useful symposium. Where to Implement the Toric IOL by Dr. Peter Hoffman from Frankfurt-Am-Main, Germany, was a real highlight.
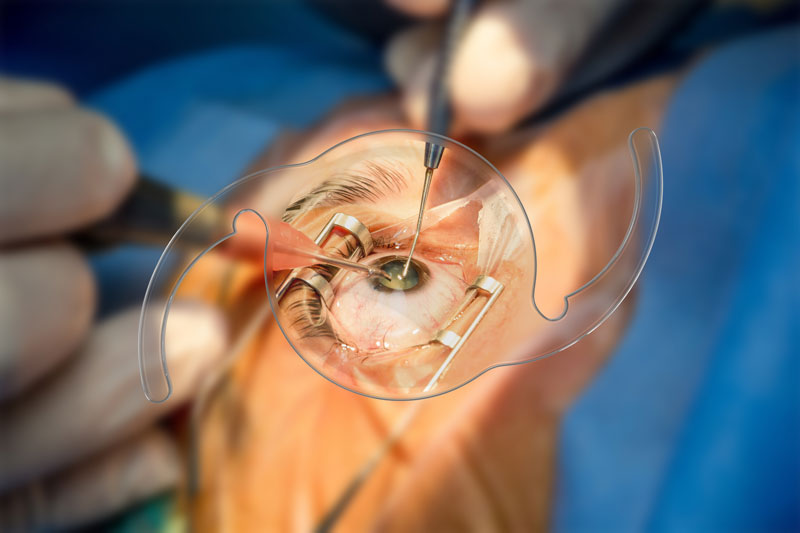
High quality IOL footage always makes us happy.
The presentation covered intraocular lenses (IOLs), naturally, but also astigmatism, and Dr. Hoffman postulated his view that surgically induced astigmatism must be avoided at all costs during toric IOL surgery. He made two recommendations as part of his presentation, the first being that in patients with low tolerance to astigmatism one should “go for” aggressive toric IOL indication, characterized by multifocal IOLs. In patients with a higher tolerance to astigmatism one should adopt a “more feeble” toric IOL approach with a monofocal IOL.
Lenses of another sort always attract our attention, which was why we particularly enjoyed the Surgical Video Symposium. The footage presented during this event was a feast for the eyes, with Dr. Jacek Szaflik’s lecture, Exchange of the Calcified IOL: The Ways to Go, providing some incredible close up shots of IOL replacement surgery. This section is well worth a watch on demand and included questions for the audience.
The viewers watched Dr. Szaflik’s work and were then asked by him how they would approach the replacement of the lens. Choices ranged from exchanging for a one piece IOL to exchanging for a scleral fixated IOL, with a plurality opting for the one piece IOL. The footage was some of the best we have seen. Kudos, Dr. Szaflik!
The Dread of Dry Eye Charts
Now if you read our new and brilliant publication focused on optometry, COOKIE (Cool – Optometry – Optics – Kudos – Innovation – Enlightenment magazine… and of course you do because you are awesome), then you will likely have read one of our articles about dry eye disease (DED). It is a fascinating topic and given how common the condition is, ophthalmologists should familiarize themselves with it as much as possible. If you want to learn more about DED then Improving Diagnostics of Ocular Surface Disease by Dr. Carina Koppen of the University of Antwerp is the presentation for you.
Presented during the second main event symposium, Ocular Surface in Our Daily Surgical Practice, Dr. Koppen’s report covered a number of areas of DED diagnostics. She recommended the use of Tear Film and Ocular Surface Society (TFOS) Dry Eye Workshop (DEWS) II Diagnostic Methodology guidelines to diagnose DED, which involves a staged approach beginning with triage questions designed to ‘rule in’ DED. Dr. Koppen admits the complicated chart of this approach can seem ‘intimidating’, but that it should not be.
The recommended diagnostic tests under the TFOS/DEWS II approach include a slit lamp examination plus tear breakup time (TBUT), tear osmolarity and ocular surface staining. Dr. Koppen also recommended always looking for meibomian gland dysfunction, a chronic diffuse abnormality of the meibomian glands. She concluded by recommending new DED diagnostic tools including meibography and interferometry of the lipid layer.
Day two of the ESCRS Winter Meeting fully lived up to its potential and we look forward to more scintillating symposium and funky footage tomorrow. We will be there again to cover the live events and to examine some of the conference’s outstanding posters and on-demand publications. Until then, as a certain anchorman would say, stay classy ophthalmology.



