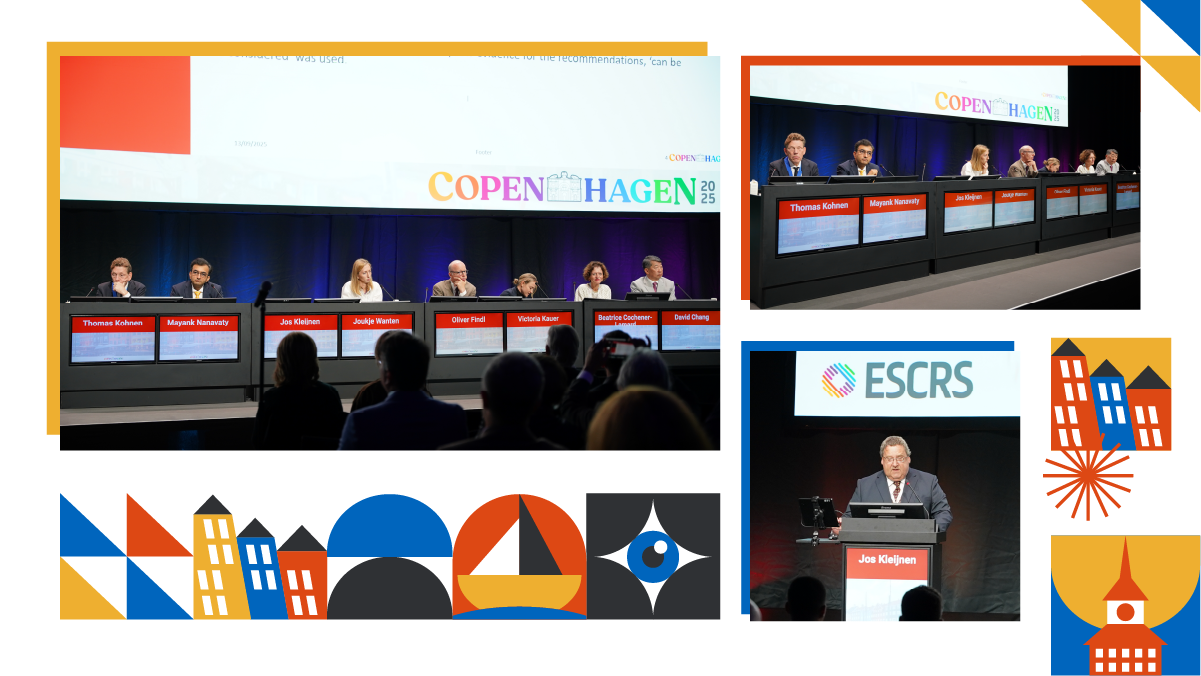
At ESCRS 2025, experts presented evidence-based strategies, spotlighted unresolved ‘grey zones,’ and emphasized the need for shared decision-making and sustainable practices.
First speaker of the session Dr. Jos Kleijnen (United Kingdom), a retired guideline methodologist, detailed the structured methodology behind the ESCRS Guidelines. He stated, “the methods and processes need to be quite structured.” The process, designed to fulfill criteria from the Appraisal of Guidelines, Research and Evaluation (AGREE) checklist, involved a development group of experts and PhD students.
They formulated questions using the PICO format (Participants, Interventions, Comparators, Outcomes) and selected relevant outcomes. The dominant system for assessing evidence was the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework, which determines the level of evidence from “high to very low.”
This systematic approach ensures transparency and reflects evidence strength, guiding clinicians appropriately while highlighting areas needing further research.

READ MORE: Opening Ceremony & Binkhorst Medal Lecture: Vikings, Vision and a Short-Sighted World
Cataract guidelines from screening to post-surgery
Next speaker Dr. Joukje Wanten (The Netherlands) highlighted the methodology behind the ESCRS Guideline for Cataract Surgery, emphasizing that they are “evidence-based, patient-centered and aim to standardize practice and increase patient safety.” She mentioned that the guidelines cover a patient’s entire journey, from screening to postoperative care, with each recommendation developed using the GRADE framework.
As Dr. Wanten stated, “Each section, each topic, starts with a review question,” ensuring structured evidence synthesis. Key recommendations include the use of intracameral antibiotic injections to prevent endophthalmitis, prophylactic non-steroidal anti-inflammatory drug (NSAID) drops to reduce cystoid macular edema (CME), and consideration of immediate sequential bilateral cataract surgery (ISBCS) for suitable patients. The guidelines also emphasize mental health, cost-effectiveness and individualized care for patients with comorbidities, reflecting a comprehensive, patient-focused methodology.
WATCH NOW: Why go dropless with OMIDRIA?
Meanwhile, ESCRS Past President Prof. Oliver Findl (Austria) explored the “grey zones” in cataract care—areas where evidence is weak and clinical practice varies. He noted that while some recommendations are supported by strong data, many everyday decisions rely on low-quality evidence and must be individualized.
“Much of what we do is based on low-level evidence,” he remarked, stressing the importance of careful clinical judgment. Preoperative assessment for presbyopia-correcting intraocular lenses (IOLs), for example, requires thorough screening for dry eye, realistic patient expectations, and detailed imaging such as topography and optical coherence tomography (OCT).
READ MORE: Optovue Solix OCT/OCT-A: Bringing High-Definition Clarity to Your Diagnostic Toolkit
Prof. Findl highlighted evolving classifications of IOLs—from monofocal and enhanced monofocal to extended-depth-of-focus (EDOF) and multifocal lenses—based on objective defocus-curve analysis. He also reviewed uncertainties around toric IOL thresholds, management of Fuchs endothelial dystrophy, keratoconus calculations and target refraction. Evidence remains limited for “dropless” cataract surgery, remote postoperative monitoring and prophylaxis to prevent cystoid macular edema, he noted, adding that ongoing ESCRS trials aim to clarify these issues, underscoring the need for shared decision-making and more randomized studies to guide practice.
READ MORE: Peering into the Future of IOLs: Enhanced Monofocals to Refractive EDOF Designs
Refractive guidelines for safer vision correction
Turning to refractive surgery, Dr. Victoria Till (Vienna) introduced the ESCRS Guidelines aimed at guiding patients, clinicians and stakeholders through evidence-based recommendations. “The purpose of this project was to establish a set of evidence-based recommendations that address both the agnostic and therapeutic aspects of reproductive surgery,” she said.
She explained that the guidelines follow the patient journey from screening and preoperative assessment through perioperative procedure, postoperative care and complication management, ensuring surgery is performed “safely, predictably and consistently.”

According to Dr. Till, the document defines outcomes across four key dimensions—efficacy, predictability, stability and safety—to provide a structured way to compare results in practice and research. It details procedure-specific parameters and safety limits for surface ablation (photorefractive keratectomy or PRK), laser-assisted in situ keratomileusis (LASIK), small incision lenticule extraction (SMILE), phakic IOLs and refractive lens exchange (RLE), noting when each is most suitable and where evidence remains limited.
READ MORE: Electrochemical Corneal Reshaping Emerges as a Potential Alternative to LASIK
Dr. Till also highlighted the importance of individualized assessment in borderline cases, stressing that “rigorous patient selection, adherence to strict procedural safety limits and realistic counseling” are essential for optimal outcomes and long-term visual quality.
Like cataract surgery, refractive surgery has its own grey zones, where high-quality evidence is limited and expert consensus is essential, acknowledged Prof. Béatrice Cochener-Lamard (France).
“The gray zones persist despite many advances, and shared decision-making is just vital,” she said, noting how the panel even debated basic definitions such as thresholds for low, moderate and high myopia, hyperopia and astigmatism. She emphasized that surgical decisions must integrate corneal morphology, patient history and patient needs, not diopter numbers alone.
Across techniques, she highlighted promising options like combined PRK–crosslinking or topography-guided LASIK, but repeatedly cautioned that long-term safety and efficacy data remain scarce. She concluded that shared decision-making, meticulous informed consent, and careful documentation are vital until stronger evidence allows today’s consensus statements to mature into formal guidelines.
The global perspective: Lessons from around the world
Offering an international outlook, Dr. David Chang (United States) traced the history of clinical guidelines, noting that the first American Academy of Ophthalmology’s Preferred Practice Patterns (PPP) in 1988 was designed “to standardize the best practices to improve outcomes, to promote cost effectiveness and to help with policy and advocacy.”
Dr. Chang noted the growing adoption of intracameral antibiotics in North America and Asia, with recent large-scale studies providing strong evidence for their effectiveness in reducing endophthalmitis, while cautioning against unnecessary use of topical antibiotics.
READ MORE: Flaps, Flares and Freaky Corneas: Navigating Refractive Complications at ESCRS 2025
He also discussed the ISBCS practice, noting its higher adoption in Asia Pacific compared to North America where financial and regulatory disincentives remain. In conclusion, he urged greater environmental responsibility, highlighting a “regulatory paradox” in the U.S.— rules that generate more waste and higher costs without better outcomes—contrasted with the efficient, safe and highly sustainable practices in India.
By combining rigorous methodology with international insight, the ESCRS Guidelines highlight both what we know—and what remains uncertain—across cataract and refractive surgery. As Dr. David Chang reminded delegates, strong data should drive practice, but sustainability and common sense must also guide the rules we follow. With ongoing registries and new trials underway, these living documents will continue to evolve, helping surgeons deliver safer, more effective and more responsible care for patients worldwide.
Editor’s Note: The 43rd Congress of the European Society of Cataract and Refractive Surgeons (ESCRS 2025) is being held from 12-16 September in Copenhagen, Denmark. Reporting for this story took place during the event. This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.