March 6-12 of 2022 is a special week in the eye world — it’s World Glaucoma Week, a week which features all sorts of information on glaucoma. The goal is to encourage people worldwide to have regular eye exams, especially covering the optic nerve, with their eye doctor to prevent and detect glaucoma. Treating the condition as early as possible can prevent long-term damage, up to and including vision loss and blindness. Glaucoma is poorly understood by the general population worldwide, so we thought we’d try to be helpful by preparing a primer for patients to understand the differences between open vs closed angle glaucoma.
Generally, and as astute readers may have already gathered, there are two types of glaucoma: open-angle glaucoma and closed-angle glaucoma, the latter of which may also be called angle-closure glaucoma. While they’re different conditions, they’re both caused by increased intraocular pressure (IOP), i.e., eye pressure. There are other, less common types of glaucoma that we’ll discuss as well.
For reference, glaucoma is an unfortunately common eye disease, and is the second leading cause of blindness in the world. Upwards of 70 million people worldwide suffer from the condition, but more treatments are emerging every year.
Many glaucoma sufferers are unaware they’re even afflicted with the disease, which is why an awareness week like this one is so valuable. Sharing information like this article can help reduce the prevalence of the disease or, at least, encourage people to seek check-ups and treatment.
So, whether you’re an ophthalmologist looking to share information with patients or a patient looking for information, this piece is for you. We’ll cover the basics of both forms of glaucoma, their symptoms, causes and potential treatments. Ready? Let’s dive in.
Glaucoma overview: Terms and conditions
Readers unfamiliar with the intricacies of the eye may wonder just what is meant by “angle.” The angle of the eye is the spot between the iris — the colored part of the eye — and the cornea, the eye’s clear protective layer. Aqueous humor, the fluid in the eye that maintains the eye and is constantly produced and removed, drains from this angle via the trabecular meshwork. Together, the trabecular meshwork and the uveoscleral drain allow for aqueous humor to properly drain from the front of the eye, a process called outflow.
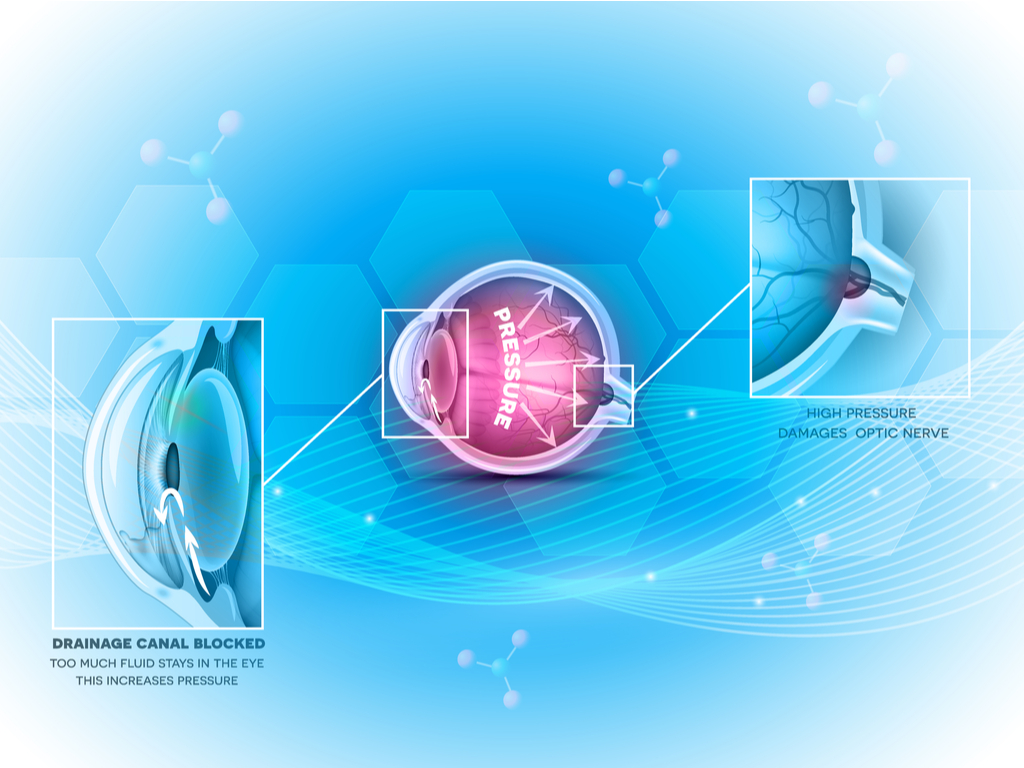
Maintaining the proper amount of aqueous humor is crucial to eye health and maintaining IOP. Open-angle glaucoma results when eyes cannot properly drain fluid via the drainage angle, which becomes clogged. This leads to eye pressure buildup, which leads to glaucoma.
Given enough time, this pressure buildup will lead to damage to the optic nerve head, found at the back of the eye. It’s this optic nerve damage that’s the dangerous part of glaucoma, and that can lead to vision loss and blindness.
Closed-angle glaucoma is less common, and potentially more dangerous, as it is caused by the malfunctioning of both drainage canals. Serious cases of closed-angle glaucoma, which can occur very suddenly, can lead to a rapid degradation of vision and can represent a medical emergency.
Let’s check out open-angle glaucoma more closely, followed by angle-closure glaucoma. Then we’ll cover risk factors and treatments.
Open-angle glaucoma: The most common type
Of the two types of glaucoma, open-angle glaucoma is the more common type of glaucoma, accounting for north of 80% of cases. It can also be called primary open-angle glaucoma (POAG).
Because open-angle glaucoma is a gradual process, many people won’t even be aware they’re suffering from the condition until they experience notable vision loss. It’s for this reason that regular eye check-ups are so valuable, since they can catch IOP problems in the early stages before they spiral out of control.
Monitoring IOP can be done with a regular visit to an optometrist or ophthalmologist, and can even be done at home with some new, nifty gadgets.
Open-angle glaucoma symptoms
As we’ve mentioned, many open-angle glaucoma sufferers won’t even know they have the condition until they’ve experienced vision loss. But indeed, reduced vision — especially peripheral vision loss — is one of the most common symptoms of open-angle glaucoma.
Other common symptoms include a swollen cornea, pupil dilation that doesn’t adequately respond to changes in light, redness in the sclera (white part of the eye) and even seemingly unrelated conditions like nausea.
What causes open-angle glaucoma?
We know that the improper functioning of the trabecular meshwork — spongy tissue that helps aqueous humor drain — is the cause of open-angle glaucoma. However, it’s not clear just why this happens in many cases. There is certainly some genetic component, as people whose parents or grandparents have had glaucoma are more susceptible to it than those with no family history of glaucoma. This is known as congenital glaucoma, and while scientists are definitely on the case, we’re not sure why this happens yet. Because glaucoma is such a multifactorial condition, much about the condition remains a mystery.
Risk factors for open-angle glaucoma include increased age, African heritage, myopia, low blood pressure, and more. The African heritage bit is particularly eyebrow-raising, as people of sub-Saharan African descent are four to eight times more likely than those of European descent to develop glaucoma. It has been suggested this is because Africans typically have thinner corneas than people from other corners in the world, but this idea is still a work in progress.
Closed-angle glaucoma
Like open-angle glaucoma, closed-angle or angle-closure glaucoma involves a degradation of the trabecular meshwork. Unlike open-angle glaucoma, however, angle-closure glaucoma also involves the uveoscleral drain — which is blocked by the “angle” being closed. In the anterior chamber (front of the eye), the iris presses against the cornea, which leads to the blockage and a narrower angle. See? The name makes perfect sense.
The most aggressive form of closed-angle glaucoma, acute angle-closure glaucoma, can come on very rapidly. Indeed, the speed of its onset is what gives it its name. It can lead to a sudden, dramatic rise in IOP that constitutes a medical emergency. Left untreated, acute angle-closure glaucoma rapidly leads to optic nerve head damage, producing vision loss and even blindness.
Closed-angle glaucoma symptoms
Symptoms of closed-angle glaucoma come on much faster and stronger than those of POAG. These can include a headache and severe eye pain, nausea, blurred vision, eye redness and halos in the vision. If you or anyone you know is having these symptoms — and you’re certain it’s not from a hangover — get to a doctor right away.
Closed-angle glaucoma risk factors
The risk markers for angle-closure glaucoma are quite different from those of POAG. For example, people of Indian or east Asian heritage are more likely to experience angle-closure glaucoma than others. Additionally, women, people with small eyes, and those experiencing high blood pressure are more at risk of the condition than the general population. Just why, yet again, is poorly understood.
Other types of glaucoma
Because glaucoma is best considered a family of diseases rather than one specific disease, there are many subsets of the condition. These can include:
- Normal-tension glaucoma, in which the optic nerve is damaged even though IOP is not elevated. This condition is poorly understood.
- Secondary glaucoma, in which glaucoma results from another factor that raises IOP above normal levels.
- Traumatic glaucoma, which results from damage to the eye.
- And several more. For more information on these specific cases, check here.
Glaucoma treatments
Treating glaucoma is one of the primary functions of the entire field of ophthalmology, so you can rest assured there are not only thousands of doctors worldwide focusing on the condition, but also entire departments of the medical industry. Because it’s such a common condition, there’s a lot of research and money invested in treatments.
The most common treatment is IOP-lowering eye drops. These will be prescribed by your eye doctor and will need to be regularly used over a long period of time. One major problem doctors and patients encounter is lack of adherence to these eye drops, simply due to patients forgetting to use them or not liking to. So, while drops are a common treatment, they have the whole “human error” factor involved.
Cataract surgery consistently leads to lower IOP, as the lens is extracted from the eye and replaced with an intraocular lens. Some doctors even suggest removing the lens in patients who don’t suffer from cataracts, but this is a somewhat controversial procedure.
Iridotomy is another common treatment. With modern laser treatment, for example, a hole is poked in the iris, allowing fluid to drain more easily.
Trabeculectomy is another procedure that lowers IOP, and one often favored by ophthalmologists. It’s a treatment that has been around for a long time and is often considered the gold standard for IOP reduction. Another trabecular-targeting procedure is laser trabeculoplasty, which has made significant strides lately in the form of selective laser trabeculoplasty (SLT).
Many other treatments are in the works, as minimally-invasive glaucoma surgery (MIGS) options like shunts in the Schlemm’s canal are becoming more popular. Other shunts and drainage devices are hitting the market, like surgical implants that reduce IOP by improving drainage via the back of the eye.
Cannabis has also been a long-used glaucoma treatment, and indeed shows significant promise as an at-home (not at-work, most likely) treatment.
One thing is for sure: More and more glaucoma treatments will become available over the next decade. Because the eye condition is so common, there’s a lot of work to be done — but progress happens one patient at a time.



