For such a small (literal) surface, there sure are a large number of nasty conditions that can cause trouble for the cornea. On Day 1 of the annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS 2022), cornea specialists convened for the Corneal Essentials symposium with updates in diagnosis, management and treatment for ocular surface conditions.
A Dab of Dry Eye
In 2022, there are plentiful options for treating dry eye, said Dr. Sumit Garg from the Gavin Herbert Eye Institute at the University of California, Irvine, during his talk on What’s the Latest in the Management of Dry Eye, MGD and Blepharitis?
So, what’s new? “We’ve had steroids for a long time and we know that they work well for dry eye but there are side effects. We have a new topical steroid in the form of loteprednol and I think we’re appreciating that dry eye is a chronic disease with these episodic flares … and these flares can happen from a variety of stimuli,” said Dr. Garg. “Now we have loteprednol 0.25% (Eysuvis) and I’ve had good results with it when I can get it covered. It’s well-tolerated by patients, I’m not so worried about pressure spikes and patients seem to like it.”
Dr. Garg briefly touched on lifitegrast and cyclosporine: “I think the newest thing with cyclosporine is that now there’s a generic version of Restasis — and what does that mean for how we access cyclosporine for our patients,” he continued.
Tyrvaya, which is a nasal spray to treat dry eye disease (DED) has also recently been launched. “This is now FDA-approved and available from Oyster Point,” shared Dr. Garg.
Another treatment he said is very useful, although probably underutilized, are thermal pulsation devices (i.e., LipiFlow, iLux, 2 MiBo ThermoFlo, TearCare).
“These work to evacuate the meibomian glands, clinical studies show that up to 86% of patients have some kind of meibomian gland disease … and when they treat it, it’s the one thing that they say makes them feel really good,” continued Dr. Garg.
He shared that he doesn’t have a lot of experience with intense pulsed light (IPL) but notes that it’s gaining popularity for dry eye indications. “I think time will tell if this becomes something we utilize more as a community.”
Other treatments in the dry eye pipeline include: Reproxalap (RASP) inhibitor, NOV03 (Perfluorohexyloctane), AR-15512 (TRPM8 agonist eye drop), AGN-231868 and AGN-242428, as well as the use of cenegermin for ocular surface (OSD) disease (which Dr. Garg noted did not meet its endpoints), keratolytic agents and the use of Dextenza for OSD.
“I certainly have a hard time identifying which patients are going to respond to which treatment — that’s frustrating for the patient and for the doctor, so hopefully with some of these new treatments, we’ll have a more streamlined way to treat our dry eye patients,” concluded Dr. Garg.
Allergies, or Something More Nefarious?
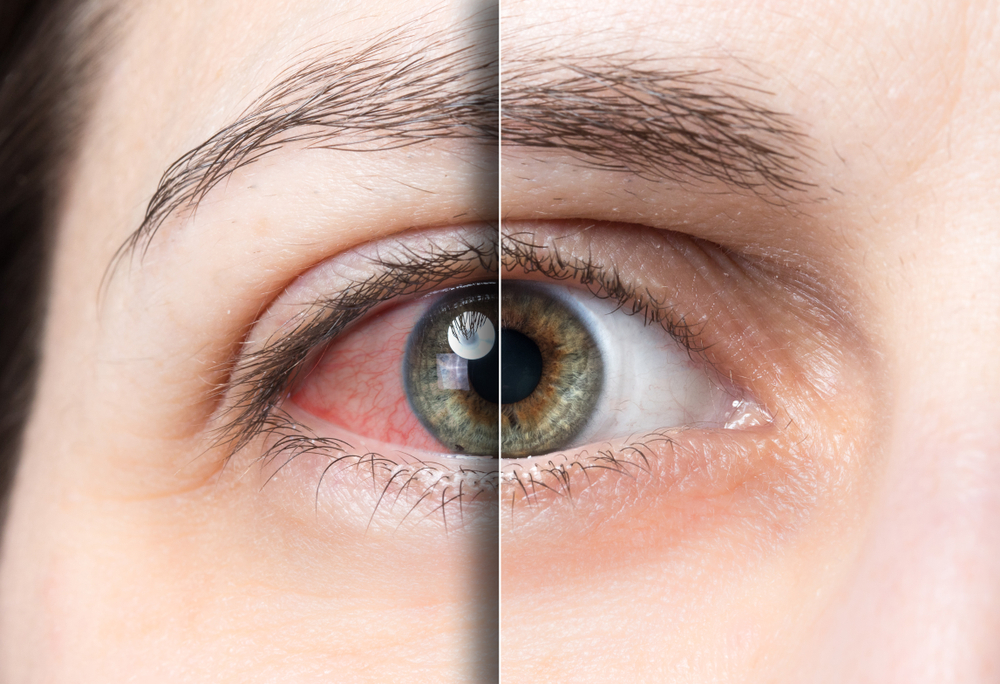
Next, Dr. Soroosh Behshad from Emory Eye Center in Atlanta, Georgia, discussed how to differentiate and treat red eyes from allergic conjunctivitis, episcleritis and scleritis.
When it comes to allergic conjunctivitis, Dr. Behshad finds it helpful to break it up into four subgroups: seasonal (the most common), vernal keratoconjunctivitis, atopic keratoconjunctivitis and giant papillary conjunctivitis.
“Now when it comes to episcleritis and scleritis, anatomy is very important,” he explained. “With episcleritis, the congestion of the vessels is going to be contained in the superficial episcleral vessels; whereas with scleritis, you may or may not have that episcleral congestion, but there’s definitely going to be congestion at the deep vascular plexus just anterior to the sclera.”
He said it’s important to remember that in most cases of episcleritis it’s idiopathic, while there’s usually a correlation between autoimmune disease and scleritis. “When it comes to symptoms, pain is going to be an important differentiating factor — patients with scleritis will be complaining of definite pain and photophobia, whereas in episcleritis, it’s usually non-specific and not painful.”
Regarding treatment, most cases of episcleritis will self-resolve; with scleritis, Dr. Behshad suggests an autoimmune work-up along with topical and oral NSAIDS.
Editor’s Note: ASCRS 2022 is being held April 22-26, as a physical show in Washington DC, USA. Reporting for this story took place during the event.



