Sponsored by Alcon
Trifocals, EDOFs and mini-monovision—how next-gen IOLs and strategies are redefining cataract surgical outcomes.
Cataract surgery just keeps getting better, especially when it comes to intraocular lenses (IOLs). At the recently held APAO-AIOC 2025 in New Delhi, Alcon (Geneva, Switzerland) brought together top surgeons to discuss what’s new in the IOL world and how these innovations are reshaping patient outcomes.
What patients expect (and don’t expect)
Dr. Tanya Trinh from Australia opened the discussion by pointing out something she often sees: many patients are caught completely off guard when told they have cataracts.
“I’m always surprised by the lack of awareness around cataracts,” she said. “Patients are often shocked when their optometrist tells them they’ve got one—like it’s this unexpected condition. But really, it’s just a natural part of aging that we all go through.”
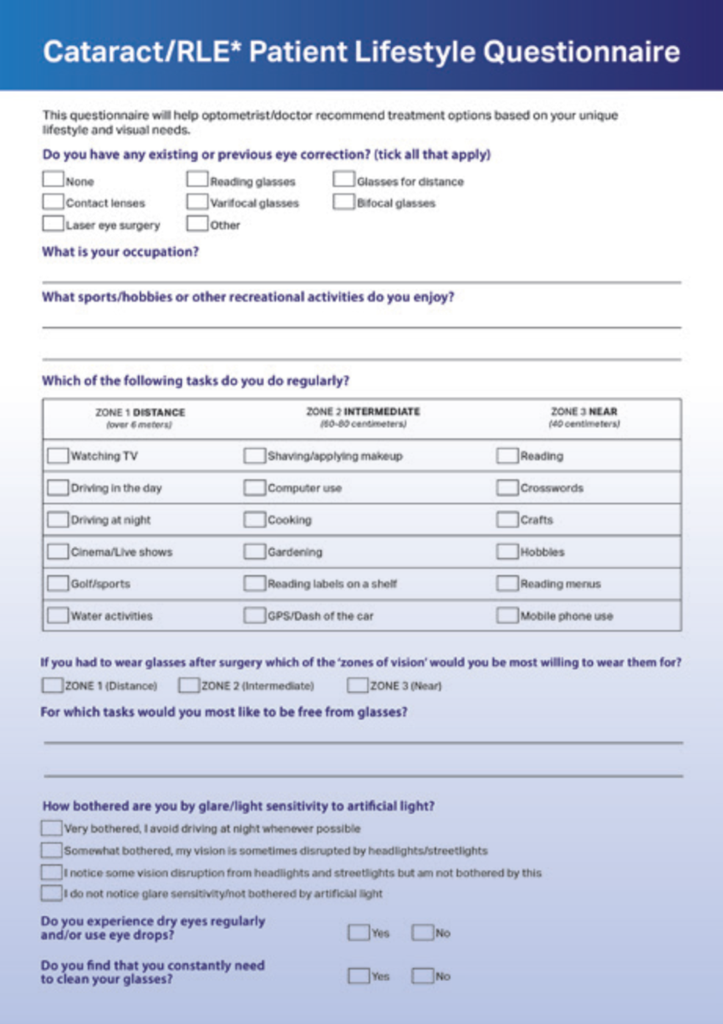
Because of this, Dr. Trinh says clear, honest conversations before surgery are key. Before recommending a lens, her team uses questionnaires to understand each patient’s lifestyle and visual needs.
“We get them to think more critically about things they normally take for granted,” she explained. “It gives us a starting point for conversations around what they might notice after surgery.”
Dr. Trinh also uses vision simulators to show patients what different lenses might look like for day and night vision, including potential glare and halo effects.

The evolution of trifocal IOLs
Prof. Thomas Kohnen, chair of Ophthalmology at the University of Frankfurt in Germany, has been working with Alcon’s PanOptix® trifocal IOLs since day one—literally. He was one of the early access surgeons in the world to implant one.
“We started using trifocal lenses in 2012,” he said. “The first iterations were made with the AcrySof® material, and now we’ve moved to the Clareon® material.”
Prof. Kohnen said that the way surgeons think about trifocals has shifted over time.
“We’re now much more reluctant not to put them in the eye,” he said. “[Especially] if they really want to be spectacle independent.”

When asked about recommending trifocal IOLs for patients with active lifestyles or who drive frequently at night—traditionally considered challenging cases—Prof. Kohnen challenged conventional thinking.
“I have really close friends who came to my department… and they love their PanOptix. They drive at night, and they go at high speeds, so that’s not a contraindication,” he shared. “The only thing is we, as physicians, have to explain it to them.”¹
The rise of non-diffractive EDOF lenses
Another major topic during the session was non-diffractive extended-depth-of-focus (EDOF) lenses—specifically Alcon’s Clareon Vivity® IOL with X-WAVE™ technology. Unlike traditional EDOF lenses that split light, this one stretches it to create a broader range of clear vision.²
Prof. Kohnen’s team published five-year data on the lens back in 2021. “We found significantly less halos in comparison to diffractive lens technology,” he recalled. “That’s a big differentiation.”³
Prof. Kohnen also sees Vivity as a great option for patients with mild ocular conditions who might not be candidates for trifocals.⁴*
“When the non-diffractive EDOF lens came on the market, I could convince a lot of them because it was closer to the monofocal lens,” he said. “Your risk of having any optical side effects is not more than with a monofocal lens.”
The surprising potential of monofocal IOLs
While premium lenses often steal the spotlight, Dr. Trinh reminded everyone not to underestimate modern monofocal lenses—especially when paired with mini-monovision strategies.
“We probably don’t give them enough credit,” she said. “They give a lot more intermediate vision… And with the right patient selection—smaller pupils, some oblique astigmatism—you can get really good results.”
In fact, Dr. Trinh pointed to studies showing that more than half of patients still report spectacle independence for distance and intermediate tasks up to three months post-op. This insight is particularly valuable for patients who may not be candidates for premium IOLs or have financial constraints.⁵,⁶**
“You don’t have to position it as ‘less than,’” she emphasized. “It’s just a different way of manipulating the optics so that we can still give patients that range of vision.”
Why astigmatism correction still matters
No matter which IOL is chosen, correcting astigmatism is a must for good outcomes, both experts agreed.
“Hayashi [et al.] have shown that residual astigmatism reduces not only distance visual acuity but also near visual acuity,” Prof. Kohnen explained. “Our goal is to measure the cornea with sophisticated devices—Scheimpflug, OCT—to get the astigmatism right.”
He added, “We rarely do astigmatic surgery on the cornea now. Occasionally, I do it, but in most cases we… manage it with the lowest amount of toricity in the PanOptix.”
Dr. Trinh also doesn’t hold back when it comes to correcting astigmatism. “As a general rule, I don’t really mind if I’m flipping in terms of the axis. I will try to aim for anything above 0.5 [diopters], and I’ll generally aim to correct that as much as possible,” she shared.
Expanding patient selection for premium IOLs
One of the most encouraging themes of the session was how newer IOL technologies—especially non-diffractive EDOFs—are broadening the pool of eligible patients.
“There is more evidence that these lenses can work for patients with early-stage glaucoma and AMD⁴*,” said Prof. Kohnen.
When asked specifically about recommending these lenses for active operating ophthalmic surgeons—traditionally perceived as challenging cases due to their high visual demands—Prof. Kohnen emphatically said, “I think these presbyopia-correcting IOLs will be ideal for these physicians because they have to look not only at the microscope, but they sometimes do other surgery which needs a larger magnification.”
Personalizing the plan
For patients who are hesitant about potential visual phenomena with trifocal lenses, Prof. Kohnen suggests a phased, custom match approach.⁷,⁸
“I’ll tell him, ‘Why don’t we do a multifocal IOL in your non-dominant eye, and wait for one or two weeks. If you really like it, we will implant your second eye, which is your dominant eye. If you really don’t like it… then let’s put Vivity in the other eye,’” he explained.
It’s a flexible strategy that gives patients more confidence and helps tailor the outcome to what feels right for them.
More options, better outcomes

These top surgeons highlighted just how far IOL technology has come—and how much more personalized cataract surgery has evolved as a result. Whether it’s advanced trifocals, innovative EDOF lens, or smart use of monofocals, patients now have more ways than ever to achieve the vision they want.
Catch the Alcon symposium on-demand here.
Editor’s Note: Reporting for this story took place during the 40th Congress of the Asia-Pacific Academy of Ophthalmology (APAO 2025), held in conjunction with the 83rd Annual Conference of the All India Ophthalmological Society (AIOC 2025) from 3-6 April in New Delhi, India.
References
- #1 trifocal lens* with over 3 million implants worldwide.† (p.81)
- Wavefront-shaping X-WAVE Technology stretches and shifts light without splitting it. (p.67)
- KOHNEN – Extended depth-of-focus technology intraocular lenses (v1.0)
- Final Vivity Registry TFLs Feb 2023 (v1.0)
- HALDIPURKAR – Evaluation of Intermediate Visual Outcomes in Eyes Implanted (v1.0)
- AGARWAL – Intermediate Vision Following Monofocal IOL Implantation (v1.0)
- IIT#76585747 – Contralateral implantation of Clareon PanOptix and Vivity (v1.0)
- LABIRIS – Mix-and-match vs bilateral trifocal & bilateral EDOF intraocular lens implantation (v1.0)
Disclaimer: For the use of recognized healthcare professionals, hospitals and laboratories only.
*The safety and effectiveness of the Clareon Vivity IOL, Vivity Toric IOL has not been substantiated in clinical trials in patients with uncontrolled glaucoma or AMD as these patients were excluded from the clinical studies. Patients with uncontrolled glaucoma or AMD may not achieve the visual acuity of patients without such conditions. As with the implantation of any IOL, careful preoperative evaluation and sound clinical judgment should be used by the surgeon to decide the benefit/risk ratio before implanting a lens in a patient with uncontrolled glaucoma or AMD.
**Product claims may vary from country to country.
© Alcon 2023 5/25 ASIA-CLI-2500013