Think trauma surgery is all blood, sweat and sutures? Think again. From 3D printing to custom irises, ASOT’s finest are turning disaster management into design thinking.
If you think trauma care is just about patching up and praying, think again.
On Day 4 at the American Academy of Ophthalmology Annual Meeting 2025 (AAO 2025), a comprehensive symposium—co-sponsored by the American Society of Ophthalmic Trauma (ASOT)—gathered some of the sharpest minds in the field to share clever, bold and sometimes delightfully rebellious ways of handling the most complex ocular injuries.
Blunt truths about TON
When it comes to traumatic optic neuropathy (TON), it seems hope and honesty must go hand in hand.
Dr. Andrew Lee (USA) kicked off his talk with a reality check. “This is the only slide you need to know,” he said, capturing the audience’s attention. “There’s no proven effective treatment yet.”


Still, Dr. Lee wasn’t all doom and gloom. He highlighted the importance of diagnosis, counseling and imaging. “Your job in traumatic optic neuropathy is to give hope,” he said, noting that the condition is a clinical diagnosis without biomarkers, and that both surgery and steroids have limited proven benefit.1
Dr. Lee outlined two surgical exceptions: canal fragments compressing the optic nerve and optic nerve sheath hematoma.
As for the future? He noted promising research on erythropoietin, though it’s still in the “watch this space” stage.
READ MORE: When AI meets Dr. Kenneth Goodman: Ethics in Focus at AAO 2025
Breaking (orbital) boundaries
You might think fixing a broken orbit is all about speed. Turns out, it’s more about strategy.
Dr. Ore-Ofeoluwatomi Adesina (USA) brought a fresh perspective to orbital floor fracture repair, challenging the long-held belief that “it’s a race against time.”
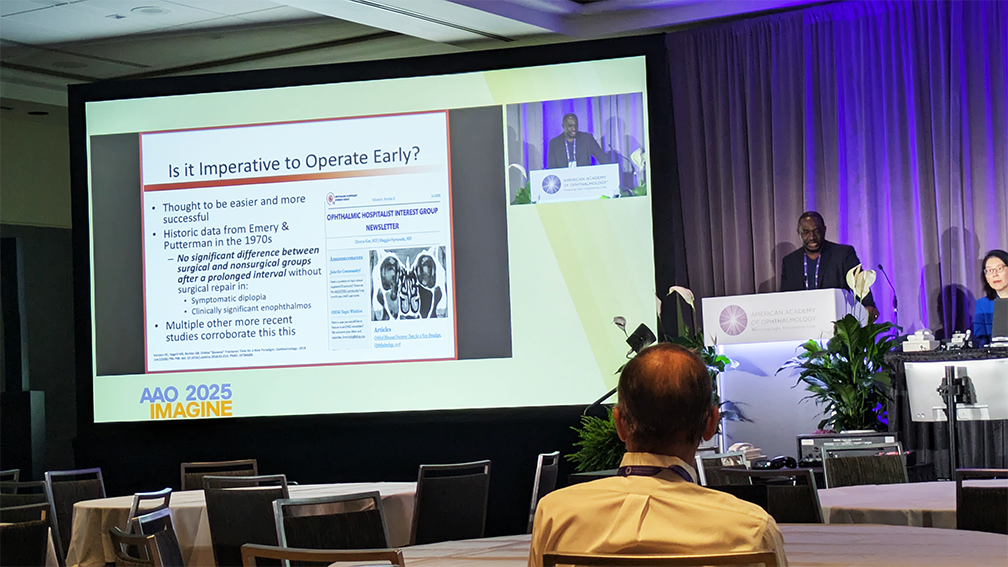

“What I was taught coming into residency was…we have to evacuate within two weeks,” he recalled. But newer research suggests delayed repairs can yield equally good outcomes, thanks to natural bone remodeling.2
Dr. Adesina then turned his focus to tech-savvy innovations reshaping fracture management. “Meta-analysis and comparative studies have shown that 3D printing can lead to improvements in orbital volume and clinical outcomes,” he shared.
Plus, according to Dr. Adesina, navigation-guided techniques and custom implants are reducing intraoperative time, bleeding and revision risk.
READ MORE: Smart Tech in Refractive Surgery
The art (and science) of iris reconstruction
Back in the days, iris repair meant old-school suturing. Fast forward to now, and it’s basically an art form.
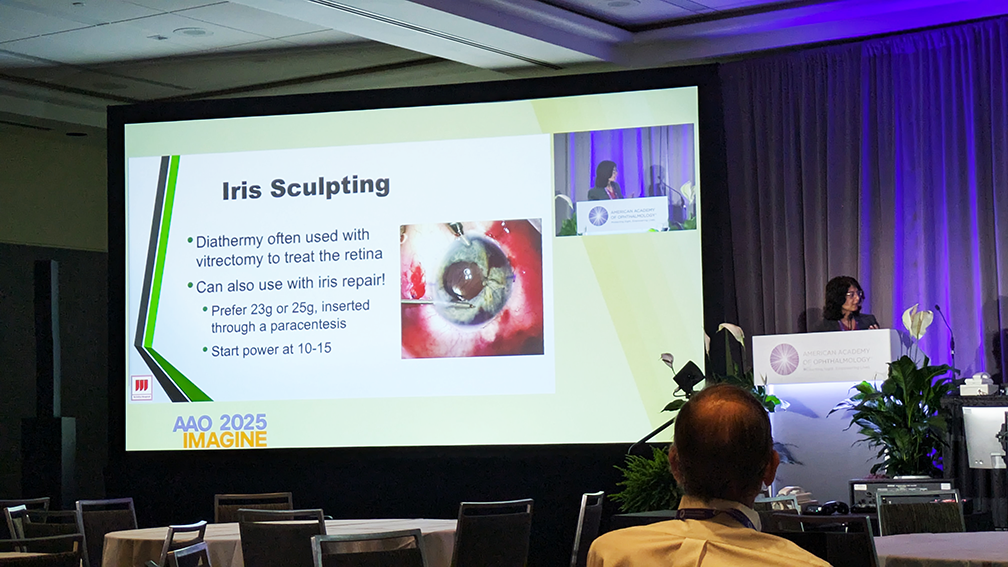
Dr. Zeba Syed (USA) recommended starting simple (iridodialysis are great training wheels) and demonstrated advanced techniques like sliding knots and “iris sculpting” with diathermy.
“Look how the iris just shrinks right there,” she narrated during a video. “You can really shrink that iris down, and now, you have a nice aesthetic round appearance rather than that kind of more distorted appearance.”
Dr. Syed also discussed the CustomFlex (VEO Ophthalmics; Ohio, USA) artificial iris, a personalized prosthetic that’s as functional as it is fashionable. “They make it custom to match the aesthetics of the other eye,” she said, noting impressive improvements in glare, light sensitivity and quality of life.
READ MORE: From Trauma to Recovery
Pediatric trauma pearls
Managing pediatric eye trauma? It’s equal parts science, speed and know-how.
Dr. Ankoor Shah (USA) distilled the latest evidence into practical pearls, beginning with standardized trauma terminology for consistency across cases.

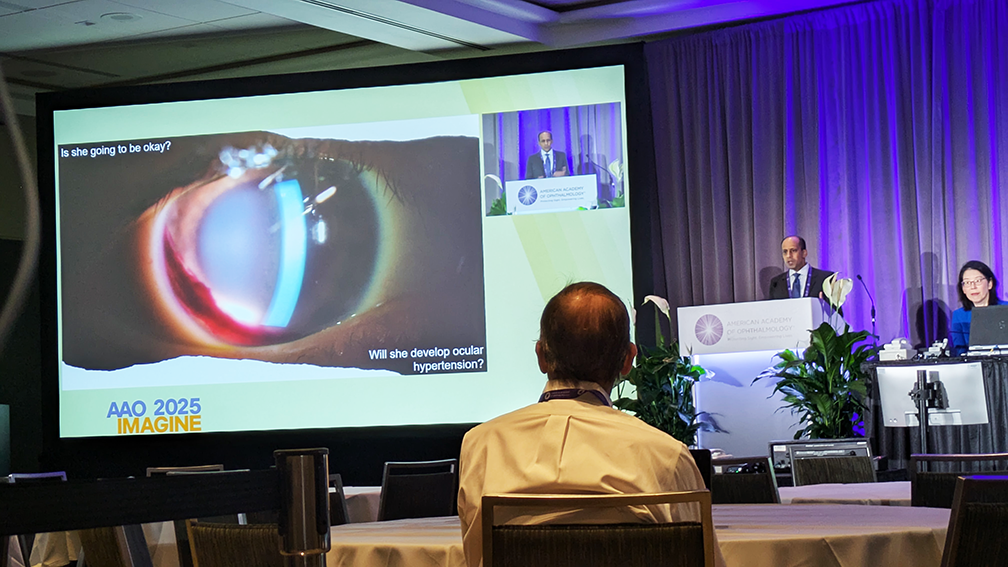
For closed-globe injuries with hyphema, he cited a study of 305 pediatric patients showing a 40% rate of ocular hypertension—most within the first week. Iris or pupil trauma tripled that risk.3
Then came his reminder on open-globe injuries: don’t drag your feet on visual rehab. “Children who develop strabismus after open globe injury had a greater median time of visual deprivation (three months) versus those who did not (one month).”
READ MORE: Management Pearls for Pediatric Ophthalmic Conditions
Glaucoma under pressure
Traumatic glaucoma is the ultimate balancing act between innovation, intuition and IOP.
Dr. Jithin Yohannan (USA) walked the audience through two complex cases that merged innovation with pragmatism. In one, a 69-year-old baseball-injury veteran underwent a hybrid approach combining complex cataract surgery and minimally-invisive glaucoma surgery (MIGS).
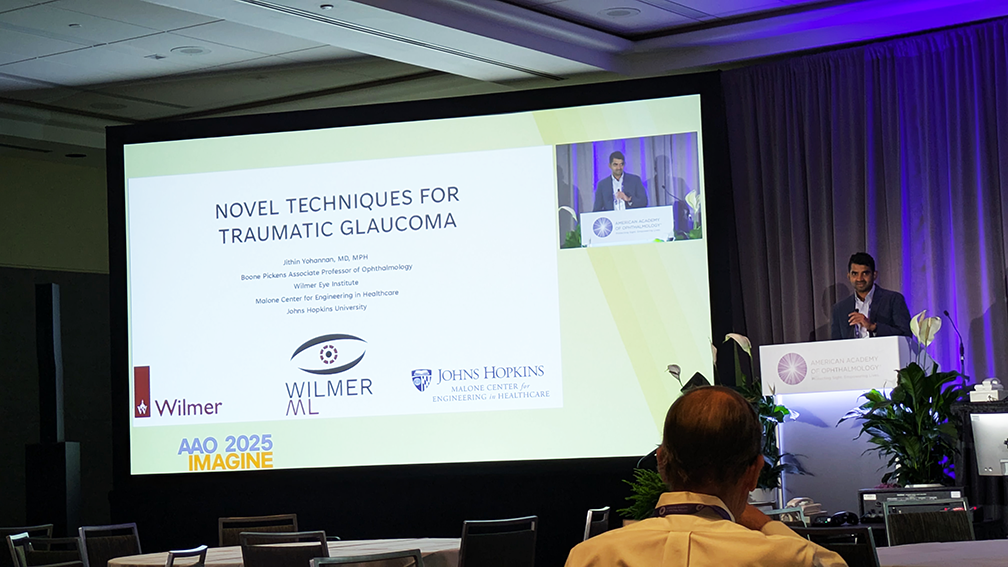
“I really like this flanged proline CTS [capsular tension segment] technique because it avoids making a peritomy, and if this guy needs glaucoma surgery in the future, we’ll be able to still use that nasal conjunctiva if needed,” he recalled.
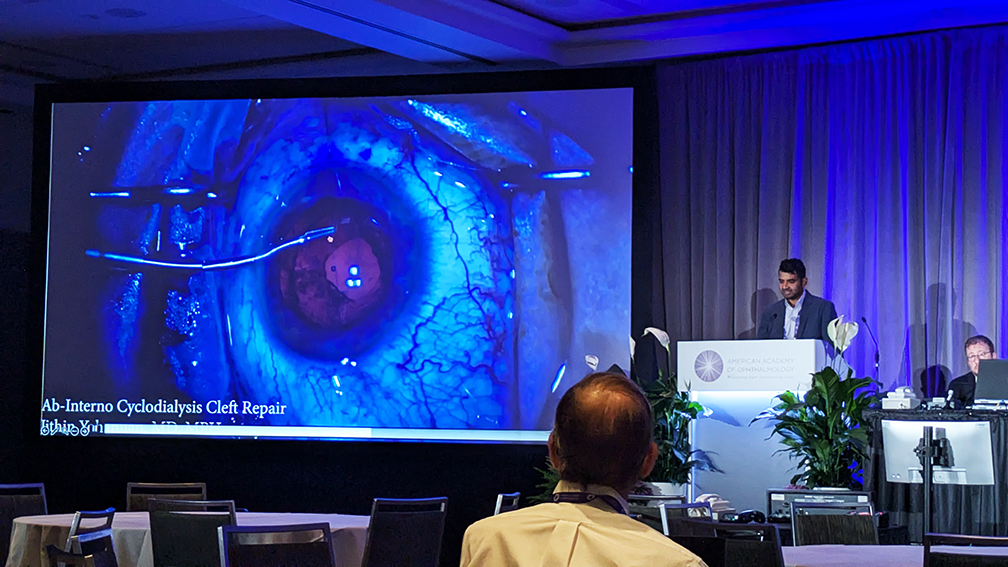
His second case dealt with a cyclodialysis cleft, a notorious troublemaker for pressure control. Using sutures under gonioscopic visualization, Dr. Yohannan managed a minimally invasive closure, though not without a warning.
“Pressures can go really high when they close,” he cautioned, noting one patient’s spike to 52 mmHg.
READ MORE: Political Posterior Surgery, Cool Cataracts & Pellet Perforations
Posterior problems, bold solutions
Posterior trauma isn’t for the faint of heart…or for those too attached to tradition.
Dr. Jules Winokur (USA) stepped up to dismantle a few sacred cows. First, the notion that all posterior scleral wounds must be fully closed. “In the attempts for complete closure, there can be excessive manipulation of the globe, which can yield prolapse of intraocular contents,” she warned.

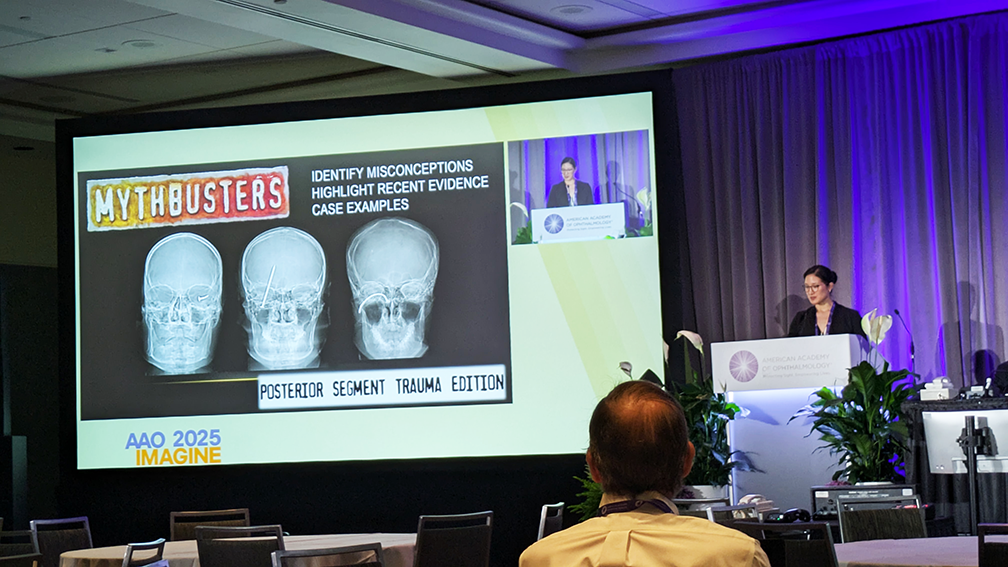
Dr. Winokur also questioned the long-standing belief that secondary vitrectomy only benefits eyes with good visual potential. “The point is, it’s really difficult to anticipate which eyes will improve significantly with secondary VR surgery,” she said, sharing a striking case where vision jumped from no light perception to 20/50.
And on the frontier of proliferative vitreoretinopathy (PVR) prevention, methotrexate is showing promise. “The GUARD trial found a significantly lower rate of redetachment with methotrexate treatment compared to historical controls,” she noted.
Innovation with impact
If trauma care once felt like a last-resort domain, this session showed that it’s now a playground for innovation.
As Dr. Jennifer Yu (USA), who co-chaired the session, reminded everyone, there’s still a nationwide need for more ophthalmologists on trauma call. And for those ready to rise for the challenge, join ASOT when they reconvene in April in Houston.
Editor’s Note: The American Academy of Ophthalmology Annual Meeting 2025 (AAO 2025) was held October 17-20, 2025, in Orlando, Florida. Reporting for this story took place during the event. This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
References
- Levin LA, Beck RW, Joseph MP, et al. The treatment of traumatic optic neuropathy: The International Optic Nerve Trauma Study. Ophthalmology. 1999;106(7):1268-1277.
- Kersten RC, Vagefi MR, Bartley GB. Orbital “blowout” fractures: Time for a new paradigm. Ophthalmology. 2018;125(6):796-798.
- Bowe T, Serina A, Shah AS, et al. Timing of ocular hypertension after pediatric closed-globe traumatic hyphema: Implications for surveillance. Am J Ophthalmol. 2022;233:135-143.
